J Int Oral Health:绝经后女性的骨质疏松状况可增加牙周病的发病率及其严重程度
2015-10-12 sunshine 译 MedSci原创
J Int Oral Health:绝经后女性的骨质疏松状况可增加牙周病的发病率及其严重程度骨质疏松症及牙周炎都是局部和全身因素介导的慢性炎症反应,其特点是骨的丧失,二者具有相同的危险因素。既往研究表明,骨质疏松症本身就是绝经妇女牙周组织破坏的一个诱发因素,但是,研究表明二者仅有中等程度的联系。本研究中,我们对比了绝经后骨质疏松妇女与绝经后但并无骨质疏松的妇女的牙周病的严重程度。研究共纳入了100
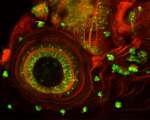
骨质疏松症及牙周炎都是局部和全身因素介导的慢性炎症反应,其特点是骨的丧失,二者具有相同的危险因素。既往研究表明,骨质疏松症本身就是绝经妇女牙周组织破坏的一个诱发因素,但是,研究表明二者仅有中等程度的联系。本研究中,我们对比了绝经后骨质疏松妇女与绝经后但并无骨质疏松的妇女的牙周病的严重程度。
研究共纳入了100名绝经后妇女,年龄在50-65岁之间。随机分组:A组,50名骨质疏松症患者;B组,50名非骨质疏松症患者。测量所有研究对象的牙周参数,包括探针出血指数,简化口腔卫生指数,牙周袋深度(PPD),临床附着丧失(CAL),邻面牙槽骨丧失(ABL)以及缺牙数。双能X线骨密度仪用以评估研究对象的牙周疾病状态与全身骨密度(BMD)之间的关系。
结果表明,与B组相比,A组女性的PPD、CAL及ABL数值更大一些(P < 0.0001)。两组BMD与牙周各参数之间并无显著相关关系。
总之,本研究结果发现绝经后骨质疏松症可增加机体牙周病的发病率,并可加重机体牙周病的严重程度。应教育绝经后骨质疏松的女性认识到良好的口腔卫生护理是自我健康管理的重要部分。因而,我们可以推断出牙周手术与牙周病之间的或可存在某种联系,但是仍需要长期的前瞻性研究以提供明确的证据。
原始出处:
Juluri R, Prashanth E et al.Association of Postmenopausal Osteoporosis and Periodontal Disease: A Double-Blind Case-Control Study. J Int Oral Health. 2015 Sep;7(9):119-23.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好文章,还会关注
88
#ALT#
61
#发病率#
61
又是系统性疾病
153
休息口腔卫生
158
#Oral#
80
#绝经#
78
#牙周病#
66
#牙周#
70
#绝经后女性#
68