近期Nash教授及其同事于JAMA Neurology杂志发表文章称,90%的复发缓解型多发性硬化(MS)患者接受高剂量免疫抑制剂以及自体造血干细胞移植后临床症状并没有缓解。该项称为HALT-MS临床研究的中期分析共纳入25例MS患者,分析结果显示无进展生存率为90.9%,无复发生存率为86.3%。
大部分严重不良反应发生在治疗后首个月内,9例患者在研究2年时出现3级不良事件,1例患者出现4级不良事件,1例患者在研究期间死亡。这些迟发性不良反应导致另一位专家在随刊评论中指出,造血干细胞移植对MS的疗效仍待进一步证实。
评论指出,“有关造血干细胞移植(HCT)的适应症尚不明确”。除了担忧干细胞治疗的安全性,评论者也开始质疑治疗是否真正有效,因为某些患者在移植术3年后其脑部病灶仍在扩大,并出现临床复发。
研究详情
研究者指出既往HCT应用于MS治疗的相关研究结果模棱两可,可能是由于患者处于疾病晚期,因此出现与非炎症性退行性变相关的持续性功能下降。HCT治疗不能逆转退行性变,但可缓解早期免疫介导的脱髓鞘病变。因此,Nash教授及其同事招募了相对早期的复发缓解型MS患者,中位病程约为5年,平均EDSS评分为4.4分,均提示患者为中等程度残疾。
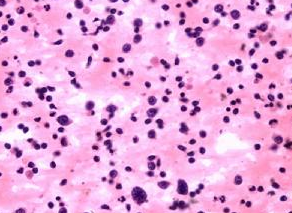
首先患者进行造血干细胞动员,紧接着是干细胞移植。然后给予由卡氮芥、依托泊苷、阿糖胞苷马法兰和抗胸腺细胞球蛋白等组成的骨髓抑制治疗方案。完成治疗的第二天,进行自体CD34阳性细胞输注,直至中性粒细胞计数恢复至500/ul 以上。同时给予强的松来预防移植综合征相关的发热。
1例患者在给药前就退出了研究,其他患者均完成了至少为期3年的随访,此时进行研究的中期分析。主要终点为治疗失败的时间,研究者规定治疗失败为:出现任何原因的死亡、临床复发、EDSS评分相较于基线变化超过0.5分以上、或者头颅MRI检查出现至少2个T2像或增强病灶。
根据上述标准,21.6%的患者治疗失败,其中复发和EDSS评分进展是主要原因。该研究中某些患者的功能也得到一定改善。随访第3年时,患者平均EDSS评分相较于基线减少0.4分,MS功能复合评分以及MS影响量表评分得到轻微改善。
研究中出现大量3-4级不良事件,所有患者均发生至少1次4级不良事件,大部分与移植治疗方案相关,就像其他疾病比如癌症治疗中所见的不良事件类似。但也有一些意料之外的不良事件,比如2例患者出现呼吸功能衰竭,2例患者出现自杀倾向。该研究计划随访5年,5年后研究者将会有一个最终的报告。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








客观评价,而不是一味的跟风
200
#多发性#
67
看看
187
#造血干细胞#
87
#造血#
61