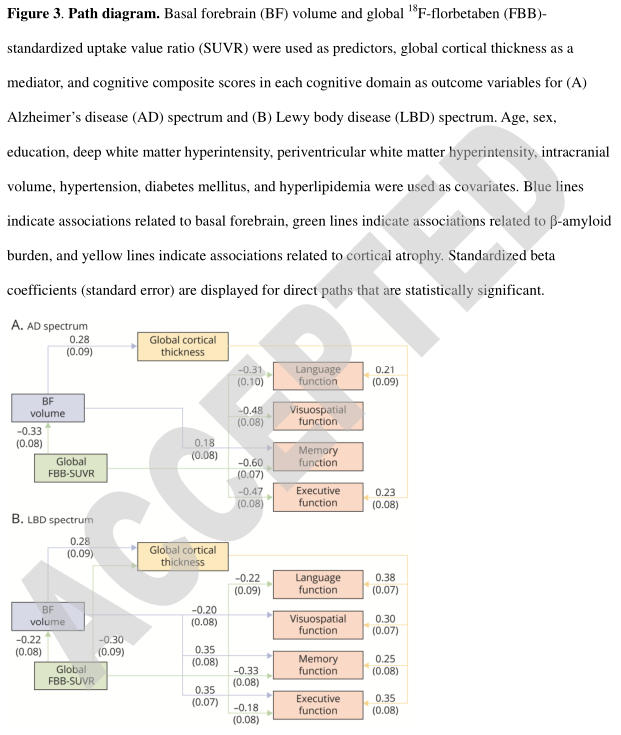
Neurology:β-淀粉样变性机制与阿尔茨海默病、路易体痴呆相关,后者共存局部性β-淀粉样蛋白和皮质萎缩相互作用
2022-01-18 Naomi MedSci原创
近日,研究人员通过神经心理学和结构功能性评估, 在AD和LBD谱中存在共同的β-淀粉样变性机制,BF萎缩与认知功能障碍的关系更为深刻,在LBD疾病谱中存在局部性β-淀粉样蛋白和皮质萎缩的相互作用。
基底前脑(BF)是中枢神经系统中乙酰胆碱的主要来源,向大脑皮层和边缘系统提供胆碱能投射,参与注意力、记忆、动机、觉醒和睡眠的调节。在神经退行性疾病中,BF胆碱能神经元通常变性,导致随后的认知功能下降。影像学和病理学证据表明,BF中胆碱能神经元的变性和皮质胆碱能神经的丧失是阿尔茨海默病(AD)和路易体病(LBD)的特征,包括帕金森病(PD)和路易体痴呆(DLB)。
在AD和AD痴呆前驱阶段,皮质β-淀粉样蛋白沉积增加与BF萎缩有关,并且BF萎缩先于并预测源于内嗅皮层的AD病理所致的皮质萎缩。在LBD中,BF易受α-synuclein病理的影响,并且胆碱能缺陷在DLB比AD更严重。几项影像学研究报告了DLB、PD和同时患有DLB和PD的患者的局灶性BF萎缩,而在DLBD中,DLB的胆碱能缺陷比AD更严重。由于皮质萎缩可以反映AD和LBD的病理扩散模式,对与胆碱能萎缩和β-淀粉样蛋白负荷相关的皮质变薄模式的比较评估有助于理解这两种最常见的神经退行性疾病。
BF核团的萎缩与AD、LBD的认知功能障碍有关。此外,BF萎缩还与皮质萎缩和β-淀粉样蛋白负荷有关,这两项都与AD和LBD的认知功能障碍有关。近日,研究人员通过认知功能评估进行神经心理学评估,通过磁共振成像(MRI)获得BF体积和皮质厚度(CTH)以及β-淀粉样蛋白负荷的18F-氟倍他滨正电子发射断层扫描进行结构功能性评估,以探究胆碱能变性、β-淀粉样蛋白与阿尔茨海默病和路易体病的脑萎缩、认知功能障碍之间的关系。
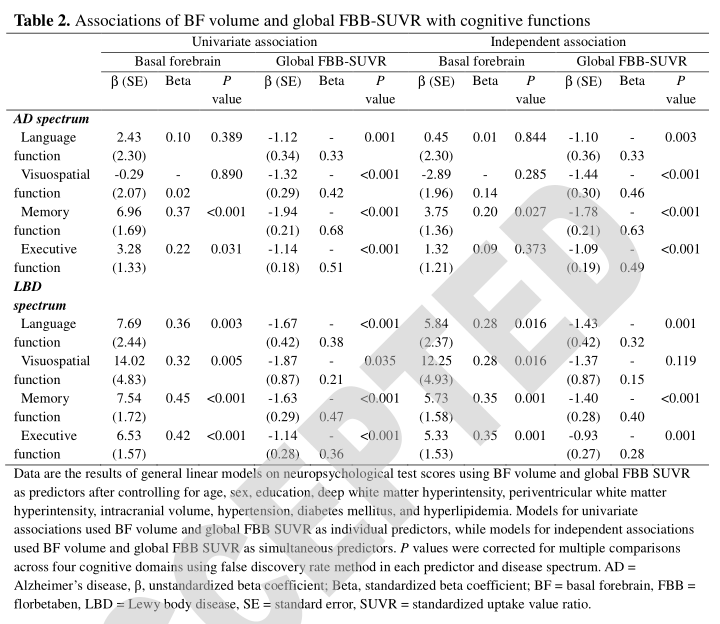
研究假设,β-淀粉样蛋白负荷和BF萎缩在疾病特异性模式中独立地导致皮质变薄,并且皮质萎缩在两种疾病中介导了两者对认知功能障碍的不同影响。
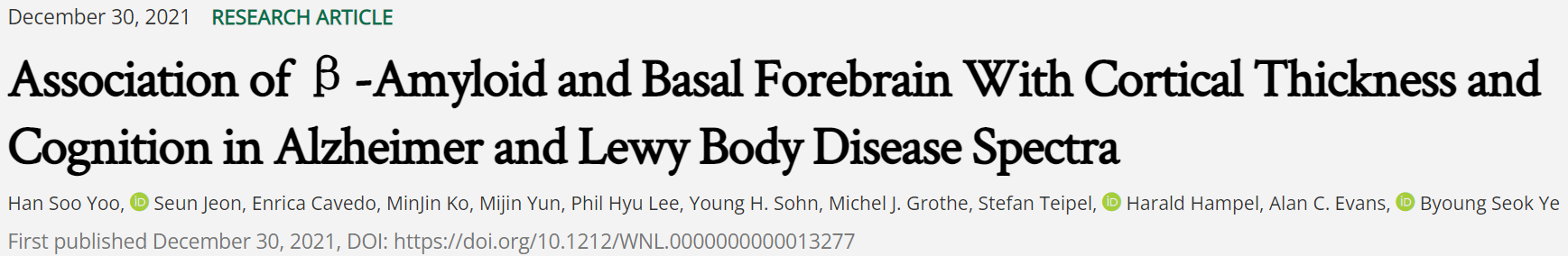
在这项横断面研究中,共招募了28名正常对照(NC)、55名AD轻度认知障碍(MCI)患者、34名AD痴呆患者、28名LBD MCI患者和51名LBD痴呆患者。对受试者进行认知功能评估,脑磁共振成像测量基底前脑(BF)体积和整体皮质厚度(CTH),18F-氟倍他滨(FBB)正电子发射断层扫描(PET)测量标准化摄取值比(SUVR)。使用一般线性模型和通径分析,分别在AD谱(AD和NC)和LBD谱(LBD和NC)中评估FBB-SUVR和BF容积与Cth和/或认知功能障碍的关系。协变量包括年龄、性别、教育程度、脑室深部和脑室周围白质高信号、颅内容积、高血压、糖尿病和高脂血症。
- BF容积介导AD和LBD疾病谱中FBB-SUVR与皮质厚度的关联,而FBB-SUVR仅在LBD疾病谱中独立于BF体积与CTH关联。仅LBD组体素FBB-SUVR与CTH显著相关。
- FBB-SUVR与AD和LBD疾病谱的广泛认知功能障碍独立相关,特别是在记忆域[AD谱的标准化β(B)=-0.60,LBD谱的标准化β(B)=-0.33]。
- 在AD疾病谱中,BF容积与记忆功能障碍相关(B=0.18),CTH与语言功能障碍(B=0.21)和执行功能障碍(B=0.23)相关。
- 在LBD谱中,BF容量和CTH与广泛的认知功能障碍独立相关。
在AD和LBD谱中存在共同的β-淀粉样变性机制,无论有无BF的介导,BF萎缩与认知功能障碍的关系更为深刻,在LBD疾病谱中存在局部性β-淀粉样蛋白和皮质萎缩的相互作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






















#相互作用#
109
#路易体#
90
#阿尔茨海#
79
#萎缩#
74
#Neurol#
83
#阿尔茨#
73
学习了。
85
在AD和AD痴呆前驱阶段,皮质β-淀粉样蛋白沉积增加与BF萎缩有关,并且BF萎缩先于并预测源于内嗅皮层的AD病理所致的皮质萎缩。
101
看看
86
#淀粉样蛋白#
97