Nature:外泌体决定肿瘤转移的器官特异性
2015-11-25 张洁/编译 生命奥秘
一项研究表明,肿瘤细胞通过释放外泌体,使受纳器官做好准备,形成转移灶。 癌细胞通过血液由起源部位传播扩散到远处器官是癌症相关死亡的主要原因。这个过程并不随机;相反,一些种类的癌症细胞会通过一系列分子程序,优先寻找特定器官,并在该处筑巢。这种寻找目的地的行为涉及到逃避原发肿瘤的癌细胞(有时也被称为“种子”)和目的器官处的微环境(或叫“土壤”)的互动。而Hoshino等人的研究发现,种子在到达之
一项研究表明,肿瘤细胞通过释放外泌体,使受纳器官做好准备,形成转移灶。
癌细胞通过血液由起源部位传播扩散到远处器官是癌症相关死亡的主要原因。这个过程并不随机;相反,一些种类的癌症细胞会通过一系列分子程序,优先寻找特定器官,并在该处筑巢。这种寻找目的地的行为涉及到逃避原发肿瘤的癌细胞(有时也被称为“种子”)和目的器官处的微环境(或叫“土壤”)的互动。而Hoshino等人的研究发现,种子在到达之前,能通过名为外泌体的胞外囊泡来影响“土壤”,从而为肿瘤转移做好准备。
越来越多证据显示,原发肿瘤转移之前会有一系列的系统性反应,这些反应甚至促使了癌症的转移。这些反应可能包括:机体血管的复杂变化、凝血和炎症——例如,癌症相关的变化包括细胞种类、可溶性蛋白和血液中外泌体的变化。
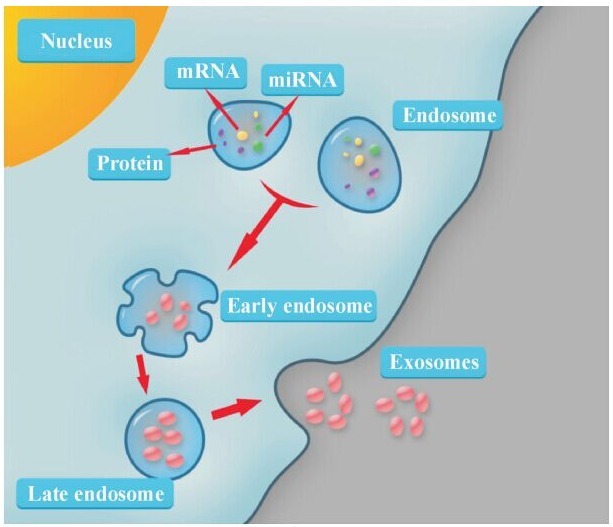
Hoshino等人把外泌体定义为小小的,把蛋白质、脂质和核酸由一个细胞运输到另一个细胞的,可以随着血液传播到远端的胞外囊泡。外泌体在癌症研究领域引起了很多人的关注——因为一些细胞外囊泡携带致癌基因,促进癌症的形成和疾病进展。
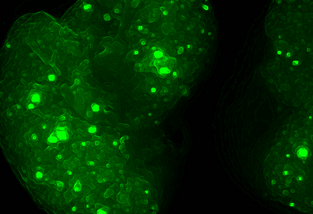
外囊泡,包括外泌体,在转移微环境形成及为转移做准备过程的几个关键事件中起了重要作用,研究者们对此也研究了好几年。例如,黑色素瘤的小鼠模型中,外泌体和毛细管壁之间的互动引起血管通透性变化,使肿瘤细胞能从血管中逃逸,进入一个新位点。此外,外泌体能把致癌基因MET受体蛋白转移到循环的骨髓细胞中,从而改变其行为,为癌症转移做准备。胰腺癌模型中,血液中的外泌体把转移抑制因子蛋白转移到肝脏的库普弗免疫细胞(Kupffer cell)上,引发一连串事件,促进转移微环境的形成。
虽然这些结果表明外泌体促进肿瘤转移,但外泌体是否和如何参与肿瘤的器官特异性转移方面的研究非常匮乏。为研究这一问题,Hoshino等人提出问题:优先转移至肺、肝、脑或骨的癌症细胞是否可能会在转移之前通过外泌体与这些器官进行互动。实验结果正是如此。把癌细胞的外泌体注射到小鼠体内,这些外泌体会滞留在癌细胞倾向于转移的器官中。此外,这些器官特异性的外泌体能与不同的细胞类型互动。例如,靶向肺的外泌体会粘附在肺内的内皮细胞上,而靶向肝脏的外泌体则会进入库普弗免疫细胞。
Hoshino等人把癌细胞的外泌体注入相同的细胞系中,证明了外泌体促进肿瘤的器官特异性转移。然后他们发现了一个有趣的现象——转移到肺部的乳腺癌细胞的外泌体能把另一类通常会转移到骨头的肿瘤细胞重定向到肺部。这一发现进一步证实肿瘤细胞的转移特征并不是自主的,而是由外部因素影响的。
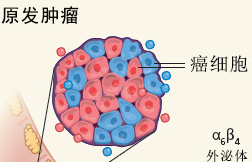
Hoshino等人针对外泌体如何影响器官特异性转移提供了几点线索。他们发现,针对不同器官的外泌体拥有不同的细胞粘附受体蛋白,即细胞表面的整合素(integrin)。不同类型的外泌体会倾向性地进入拥有大量与其表面整合素对应的配体的器官中。例如,αVβ5整合素把外泌体定向到肝脏,而α6β4则定向到肺(图1)。此外,抑制胞外体的表达或整合素的表达,能抑制癌症转移。最后,Hoshino外泌体侵入目的器官时,会引起S100蛋白的合成,从而促进炎症和细胞迁移,并激活Src蛋白——这些都为癌症细胞的转移奠定基础。

图1 为器官特异性转移做准备。a, 外泌体从原发肿瘤的细胞中释放出来,进入血液,把蛋白质、脂质和核酸运输到身体远端的细胞中。Hoshino等人发现,不同肿瘤细胞分泌的外泌体表面的整合素不同。整合素的类型决定了外泌体粘附的细胞类型。例如,整合素 α6β4 和 α6β1在肺转移中起关键作用,而整合素 αvβ5 在肝转移中起关键作用。b, 外泌体的内含物会引起目标器官的细胞变化,从而为癌症转移做准备。外泌体引导其来源癌细胞进入特定器官,促进肿瘤细胞发生器官特异性的转移和增殖。
这些重要发现扩大我们对肿瘤器官特异性转移的认识。然而,如何把这一认识转化为临床手段还需要更充分的研究。Hoshino等人证实了整合素的表达可以预测转移,指出外泌体整合素用于癌症诊断的潜能。他们的数据还表明,整合素抑制剂可能会减少特定器官癌症的转移。但在许多情况下,晚期癌症会扩散到多个器官,限制了器官特异性转移疗法的应用前景。
需要注意的是,肿瘤转移的分子通路(无论是外泌体依赖和独立的)可能非常多。因此,它们可能受很多相关因素影响:肿瘤细胞中的不同通路的激活、肿瘤中的一个特定分子亚型的出现,以及干预治疗等。例如,乳腺癌分子亚型之间的脑转移发生率不同,致癌蛋白ERBB2型乳腺癌,即使在ERBB2抑制剂有效治疗后,仍更倾向于转移到脑。科学家们不清楚的是,ERBB2抑制剂治疗是否会影响,以及如何影响器官倾向性的外泌体的释放。他们对这一课题的研究怀有极大兴趣。同样,炎症、凝血功能异常和其它癌症相关的生理变化可能会与外泌体的器官定向机制有关,因此在分析转移路径时,必须充分考虑这些因素。因此,不同类型的癌症中外泌体定向特定器官和影响“土壤”的机制还需要更充分的研究。
原文检索:Janusz Rak.et.al. Organ-seeking vesicles. Nature, 527(1038): 312-313.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好复杂的机制
84
很好,不错,以后会多学习
73
外泌体与微环境中的炎症细胞,纤维母细胞相互作用值得研究。癌症常常伴发纤维母细胞的增生及炎症反应。
79
涨知识了,谢谢分享
94
外泌体用动物模型才能做吗
86
外泌体
54
谢谢分享学习了
54
继续学习
68
继续关注
61
学习啦,,
0