J Med Case Reports:克拉霉素“老药新用”使复发难治性多发性骨髓瘤获完全缓解!
2018-04-26 不忘初心 肿瘤资讯
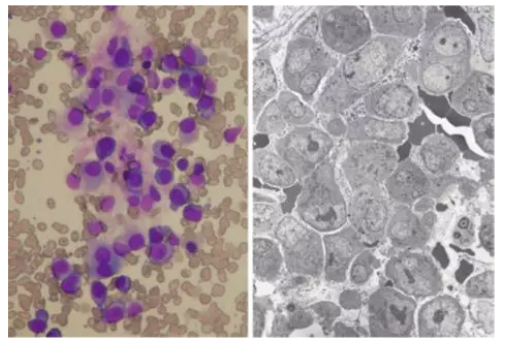
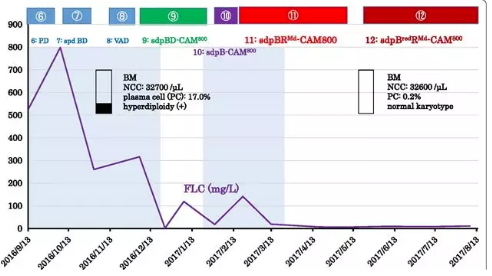
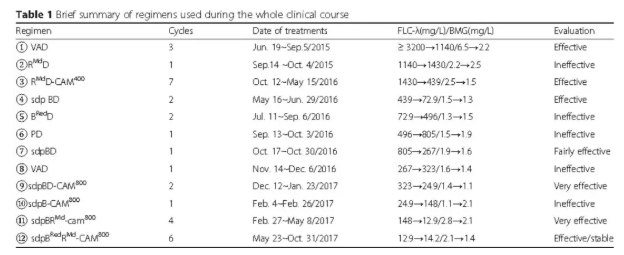
地塞米松(Dexamethasone)是治疗多发性骨髓瘤(MM)方案中的重要组成部分,疗效已被认可,但会引起各种不良反应。该个案报道介绍了一种不含地塞米松的新方案——由硼替佐米(Bortezomib)、来那度胺(Lenalidomide)联合克拉霉素(Clarithromycin)组成,治疗1例合并糖尿病(DM)的难治性λ轻链型MM,并获得了严格意义完全缓解(sCR)。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#case#
92
#case report#
66
#复发难治#
62
#多发性#
66
#完全缓解#
66
#难治性#
0
#Med#
45
#Cas#
49
谢谢分享学习
96
^_^^_^^_^
74