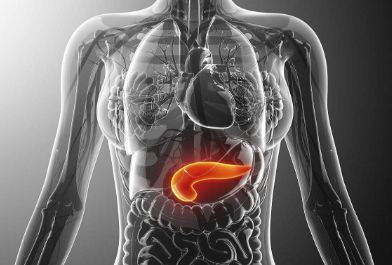
Sci Rep:一个评估主动脉瓣狭窄患者预后的新型非侵入性指标
2020-05-27 xiangting MedSci原创
在保留LVEF的中重度AS患者中,dσ*/dtmax<2.8s-1与不良临床结局独立相关。
左心室(LV)整体收缩指数,dσ*/dtmax测量了压力标化LV壁应力的最大变化率。这项研究旨在描述不同严重程度并保留左心室射血分数(LVEF)主动脉瓣狭窄(AS)患者的dσ*/dtmax趋势,以及在中重度AS患者中dσ*/dtmax与临床结局之间的关系。
这里回顾性研究了2001年1月1日至2015年12月31日诊断的1738例AS患者(550例轻度,738例中度,450例重度),这些患者保留LVEF≥50%。尽管保留LVEF,但dσ*/dtmax随着AS严重程度的增加而恶化(轻度AS:3.69±1.28s-1,中度AS:3.17±1.09s-1,重度AS:2.58±0.83s-1,p<0.001)。dσ*/dtmax<2.8s-1与主动脉瓣置换、充血性心力衰竭住院和全因死亡率复合结局的风险较高相关(调整后危险比1.48,95%CI:1.25-1.77,p<0.001)。
总之,尽管保留了LVEF,但dσ*/dtmax随着AS恶化而下降。在保留LVEF的中重度AS患者中,dσ*/dtmax<2.8s-1与不良临床结局独立相关。
原始出处:
Hui Wen Sim. A new non-invasive index for prognosis evaluation in patients with aortic stenosis. Sci Rep. 30 April 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者预后#
71
#侵入性#
0
#非侵入性#
69
#主动脉瓣#
56
#主动脉#
79