JASN:肾脏疾病患者,严格控制血压更长寿
2016-08-14 fsy 译 MedSci原创
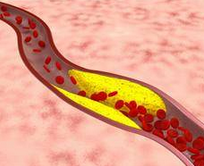
对于慢性肾脏疾病患者,严格控制血压可能有助于防止过早死亡。这是一个最近的临床试验数据的分析得出的结论。这一发现刊登在即将发行的美国肾脏病学会(JASN)杂志上。血压治疗目标是一个持久辩论的主题。近些年一些随访患者几年的临床试验已经表明,当收缩压较低,为<120mm Hg时(低于目前推荐的目标),对于心脏健康和长寿是有益的。另一方面,一些长期观察研究表明,降低血压水平可能是有害的。为了更好地考
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病患者#
62
#控制血压#
54
#ASN#
59
文章很好值得关注
76
赞了!深度好文,深入学习。
76
赞!好文章,拜读,深入学习。
74
很好,不错,以后会多学习
104
整的很不错的
56
不好意思,手机装在口袋里,自动重复
58
整的很不错的
0