ISC2018:Thomas Willis讲座:机制研究发现卒中治疗新靶点
2018-01-27 国际循环编辑部 国际循环
美国匹兹堡大学医学院Jun Chen教授作了Thomas Willis讲座,发表题为“Mechanistic Research to Identify Novel Targets for Stroke Therapy: The Dawn of a New Era of Integrative Approaches”的精彩演讲。现撷取精华内容,与读者共享。
当地时间2018年1月24~26日,国际卒中大会(International Stroke Conference 2018)在具有“天使之城”美誉的美国加利福尼亚州洛杉矶会议中心隆重举办。美国匹兹堡大学医学院Jun Chen教授作了Thomas Willis讲座,发表题为“Mechanistic Research to Identify Novel Targets for Stroke Therapy: The Dawn of a New Era of Integrative Approaches”的精彩演讲。现撷取精华内容,与读者共享。

美国匹兹堡大学医学院Jun Chen教授
过去四十年间,有关脑部疾病大多数研究大部分是以神经为中心,但未能改善老年患者长期临床结局。不过,过去20年间我们对卒中模型中程序性细胞死亡激活及预防机制的认识显著提高。例如,人们确定了可促进脑缺血损伤后线粒体功能障碍及细胞死亡caspase依赖性及非依赖性信号通路,发现抑制凋亡相关通路(如caspase-9或caspase-3)可减轻缺血后急性神经元死亡,但不能实现长期神经恢复。相反,遗传消融或抑制促凋亡分子如凋亡信号调节激酶1(ASK1)有助于促进长期神经恢复。此外,通过采用APE1对损伤DNA进行碱基敲除修复来提高内源性修复功能有助于保持大脑灰质及白质生存力并改善长期结局。
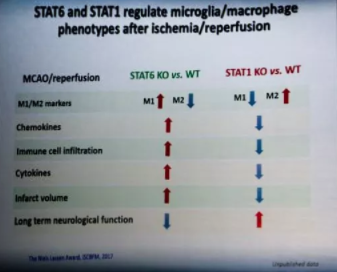
目前,有关卒中发病机制已发展到涉及神经元、星形胶质细胞、少突胶质细胞、小胶质细胞、周细胞及内皮细胞等共同组成的神经血管单位(NVU)动态相互作用。缺血时NVU的第一道防线是小胶质细胞的快速激活,进而清除细胞碎片并促进组织修复,但这也具有破坏能力、可加剧组织损伤。经典的活化M1小胶质细胞可释放破坏性促炎介质,M2小胶质细胞的激活则可通过缓解局部炎症、吞噬细胞碎片和提供营养因子来促进大脑恢复。缺血性卒中时小胶质细胞组成的连续区域可呈现极化状态,我们预计以大脑炎症为靶标的治疗方法必须从全面的小胶质细胞抑制向维持多种功能表型脑细胞之间的微妙平衡来转变。控制小胶质细胞极化的靶向内在分子开关有助于研发新的可促进脑损伤后神经血管网络恢复的治疗方法。
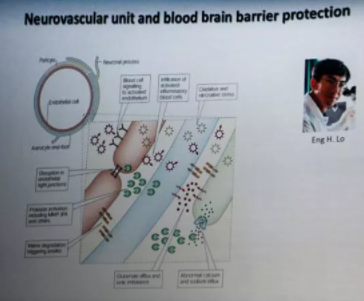
最近,NVU概念已延伸至包括了循环至大脑的血液免疫细胞。研究发现,嗜中性粒细胞、巨噬细胞、T淋巴细胞、B淋巴细胞及血小板是卒中后血脑屏障(BBB)功能障碍和NVU紊乱的关键因素。例如,系统性应用纯化的调节T细胞可显著减轻缺血性损伤,降低溶栓诱导的出血风险,并可在相对广泛的时间窗内改善长期神经结局。值得强调的,适应性T细胞发挥早期保护作用并不需要其通过BBB,而是可通过调节外周免疫细胞的有害活性来间接保护大脑。因此,调节性T细胞等外周细胞作为易于临床测量的缺血性损伤早期反应物,具有非常的大作为诊断标志物及治疗干预方法的临床转化应用潜力。

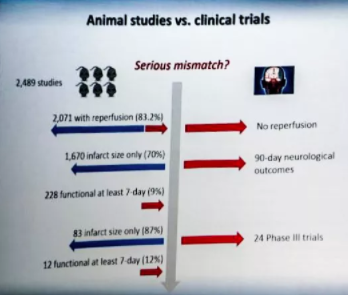
大多数有关卒中治疗的临床前研究采用缺血/再灌注模型,而临床试验则通常针对表现为无再灌注的永久性局部缺血的老年患者。但是,近期临床试验表明,更多卒中后再灌注患者有望被用于未来的研究。近年来的进展使得我们可以选择性控制蛋白质及其细胞特异性作用,极大地加深了我们对于受损NVU中蛋白-蛋白及细胞相互作用的理解。相关研究提示,我们有必要研发综合策略来同时解决神经元死亡、小胶质细胞极化、白质损失、免疫细胞入侵、DNA损伤等多个问题。遵循STAIR指南,监测长期结局、对白质及灰质中多种细胞类型进行活力评估、对伴有合并症的女性及老年患者以及多个物种进行研究以及在脑损伤后实际时间范围内进行治疗这些能均有助于改善临床前研究的预测效度。因此,我们仍乐观地认为,通过这些综合性努力所获取的机制方面的新见解将有助于加速未来发现新治疗方法的步伐。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#机制研究#
50
#研究发现#
46
诊疗进展值得借鉴
59
#新靶点#
52
#治疗新靶点#
48
#ISC#
46
阅
49