近日,一项刊登于国际期刊Nature Communications杂志上的研究报告中,来自北卡罗来纳州立大学、北卡罗来纳大学教堂山分校、和郑州大学第一附属医院的研究人员通过研究开发了一种新型人工合成干细胞(synthetic stem cells)用于治疗心肌梗死。人工合成干细胞可明显规避天然干细胞移植所诱发的可能有害风险。 此外,人工合成干细胞可耐受快速冻融,这一特性和理念可广泛应用于其他类型的干细胞。

多项研究表明,干细胞治疗主要通过旁分泌机制(释放蛋白质和核酸等)修复损伤组织。虽然干细胞治疗的有效性已得到广泛证实,但是其疗法仍具有一定的潜在风险,例如诱导宿主肿瘤形成和免疫排斥反应。另外,干细胞自身具有易碎性、难保存性、和操作的复杂性等缺点。
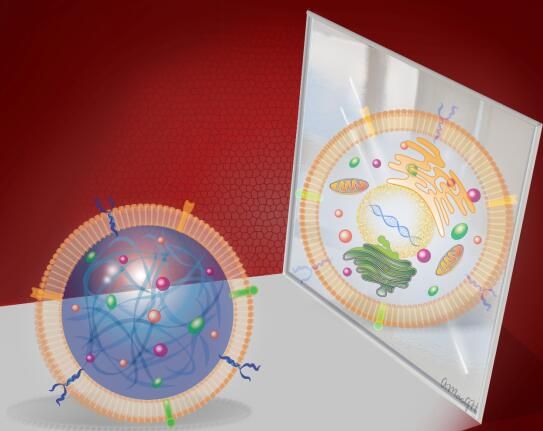
任职于北卡罗来纳州立大学和北卡罗来纳大学教堂山分校的本文通讯作者程柯Ke Cheng教授,一直致力于心脏干细胞的研究。这次,Cheng教授位于北卡的实验室和郑州大学第一附属医院的张金盈教授合作,研发出具备心脏干细胞分泌因子和细胞膜的人工合成干细胞,并命名为细胞模拟微粒(Cell-mimicking microparticle, CMMP)。
Cheng说,“我们的设计思路是从天然心脏干细胞中提取分泌因子,再和生物可降解微粒融合形成颗粒,最后包被心脏干细胞的细胞膜。我们称这种能模拟细胞治疗功能的微球为细胞模拟微粒CMMP。”
体外研究实验证明,CMMP和心脏干细胞均可促进新生乳鼠心肌细胞的生长和搏动性。研究人员在小鼠的急性心肌梗死模型上检测CMMP的治疗功能时发现,CMMP具备和天然心脏干细胞相似的心脏修复作用。由于人工合成的干细胞没有细胞核,因此降低了诱发宿主肿瘤形成和免疫排斥的风险。
Cheng介绍到,“人工合成的干细胞更像是灭活的病毒载体。其细胞膜可促使人工合成干细胞和心肌组织结合,进而释放旁分泌因子修复损伤心肌,但又可以最大程度的不诱发免疫排斥反应。所以人工合成干细胞既可以发挥干细胞的治疗作用又可规避其诱发的副作用。”
相较于天然提取和扩增的干细胞,合成干细胞具备稳定性和快速冻融的耐受性。并且合成干细胞不需要从患者自身组织中临时提取,制备过程除了适用于心脏干细胞外,同样适用于其他类型的干细胞。
Cheng期望CMMP将来可以进一步发展为商业化的药品,使更多的患者得益于干细胞治疗。论文的共同通讯作者郑州大学第一附属医院的张金盈教授同样认为CMMP的研发具有巨大的社会价值和经济价值,他表示,“目前心血管疾病是全世界范围内患者死亡的主要原因。据世界卫生组织(WHO)统计,仅2012年就有1750万人死于心血管疾病,占全球死亡总数的30%以上。因此,如何提高心血管病患者的生存率和改善预后是心血管领域科学研究的首要目标。目前临床上治疗心肌梗死疾病的手段主要局限于药物治疗和手术治疗。现阶段干细胞治疗虽然已开展临床试验,但是仍有众多局限性。人工合成干细胞的研发拓宽了干细胞治疗的领域和方式,具有一定的临床实用潜力”。论文的第一作者唐俊楠博士和共同第一作者沈德良副教授表示将继续沿用CMMP的制备理念,进一步研究CMMP的治疗机制和相关转化实验,期待有一天CMMP能应用于临床并造福患者。(生物谷Bioon.com)
Therapeutic microparticles functionalized with biomimetic cardiac stem cell membranes and secretome
DOI. 10.1038/NCOMMS13724
Junnan Tang, Deliang Shen, Thomas George Caranasos, Zegen Wang, Adam C. Vandergriff,Tyler A. Allen, Michael Taylor Hensley, Phuong-Uyen Dinh, Jhon Cores, Taosheng Li,Jinying Zhang, Quancheng Kan, Ke Cheng
Stem cell therapy represents a promising strategy in regenerative medicine. However, cells need to be carefully preserved and processed before usage. In addition, cell transplantation carries immunogenicity and/or tumourigenicity risks. Mounting lines of evidences indicate that stem cells exert their beneficial effects mainly through secretion (of regenerative factors) and membrane-based cell–cell interaction with the injured cells. Here, we fabricate a synthetic cell-mimicking microparticle (CMMP) that recapitulates stem cell functions in tissue repair. CMMPs carry similar secreted proteins and membranes as genuine cardiac stem cells do. In a mouse model of myocardial infarction, injection of CMMPs leads to the preservation of viable myocardium and augmentation of cardiac functions similar to cardiac stem cell therapy. CMMPs (derived from human cells) do not stimulate T-cell infiltration in immuno-competent mice. In conclusion, CMMPs act as ‘synthetic stem cells’ which mimic the paracrine and biointerfacing activities of natural stem cells in therapeutic cardiac regeneration.











#Nat#
43
#研发#
48
#重磅#
56
#人工合成#
59