European Radiology:冠状动脉CTA的扫描并非一成不变!
2022-02-18 shaosai MedSci原创
颈部和头部血管的CTA扫描是卒中急诊影像学的核心内容。在急性出血性卒中患者中,CTA的静脉期可以增加点征的检出率,但如果在动脉期检出斑点征,脑内血肿扩大的可能性更大。
颈部和头部血管的CTA扫描是卒中急诊影像学的核心内容。在急性出血性卒中患者中,CTA的静脉期可以增加点征的检出率,但如果在动脉期检出斑点征,脑内血肿扩大的可能性更大。
由于医院的技术设备不同(如CT扫描仪、造影剂),CTA的采集则需要制定个性化的检查方案。在日常工作中,使用个性化的CTA方案可能会导致颅内动脉期的某种变化。然而,CTA动脉期的变异性在诊断血管闭塞或异常沟通方面存在漏诊或误诊的风险,对病人护理以及研究数据的可靠性和可重复性会产生不利影响。
近日,发表在European Radiology杂志的一项研究评估了单期相CTA动脉期的变异性,为临床个性化扫描方案的制定提供了参考依据。
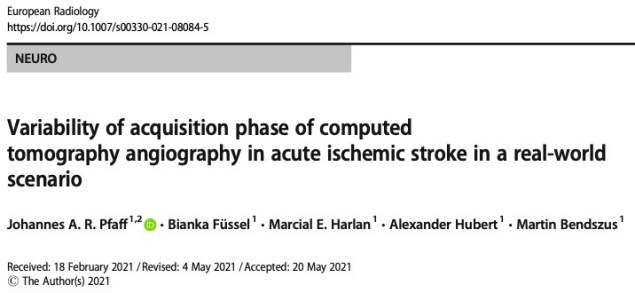
本回顾性地测量了在综合卒中中心(CSC)或八个初级卒中中心(PSC)就诊的急性缺血性卒中患者的CTA扫描的血管对比密度。CTAs被分为动脉期或静脉期,以及5个阶段中的一个(早期动脉期、动脉高峰期、平衡期、静脉高峰期和静脉晚期)。
总的来说,有871份CTA(CSC:n = 431(49.5%);PSC:n = 440(50.5%))被纳入最终分析。在Willis环的水平上只观察到较高的静脉对比密度(总体n = 13(1.5%);CSC:n = 3/431(0.7%);PCS:n = 10/440(2.3%);p = 0.09)。在CSC获得的CTA更经常显示早期动脉期(CSC:n = 371 (86.1%); PSC:n = 153 (34.8%), p < 0.01)。平衡期,即动脉稍强,静脉造影剂填充清晰,在PSC的CTA中更常见(CSC:n = 6(1.4%);PSC:n = 47(10.7%);p < 0.01)。
图 在最终分析中,根据解剖学水平每个阶段CTA研究的分布(n = 871)。*由于伪影(如移动、体外材料)导致的缺失值,无法可靠地测量HU。CTA = 计算机断层扫描血管成像。
尽管技术设备和检查方案不同,但静脉造影的CTA总体数量不多,在综合卒中中心和初级卒中中心之间没有差异。进一步区分的扫描期相之间的差异表明,CTA 采集方案有进一步改进的可能。在大型医院网络或多中心研究中,在评价CTA图像、评估图像质量和比较结果时,也应考虑颅内动脉的显示期相。
原文出处:
Dominik Laskowski,Sarah Feger,Maria Bosserdt,et al.Detection of relevant extracardiac findings on coronary computed tomography angiography vs. invasive coronary angiography.DOI:10.1007/s00330-021-07967-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#冠状动脉CT#
75
#CTA#
66
#PE#
53
学习
78