Cell Res:RANKL抑制剂有望预防乳腺癌的发生
2016-06-04 MedSci MedSci原创
大约8名女性中就有一人将在她的一生当中患上浸润性乳腺癌。这可能是使用人工合成性激素和其他环境因子导致的,也可能是BRCA1基因等发生突变导致的。平均而言,BRCA1基因发生突变的女性有高达87%的风险患上乳腺癌。截至目前,预防性手术切除是显著降低乳腺癌风险的唯一方法,但是这也经常伴随着术后并发症。 2010年,奥地利科学院分子生物技术研究所(IMBA)科学主任Josef Penninge

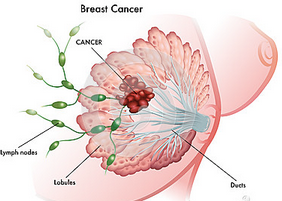
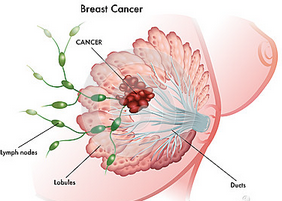
大约8名女性中就有一人将在她的一生当中患上浸润性乳腺癌。这可能是使用人工合成性激素和其他环境因子导致的,也可能是BRCA1基因等发生突变导致的。平均而言,BRCA1基因发生突变的女性有高达87%的风险患上乳腺癌。截至目前,预防性手术切除是显著降低乳腺癌风险的唯一方法,但是这也经常伴随着术后并发症。
2010年,奥地利科学院分子生物技术研究所(IMBA)科学主任Josef Penninger和他的研究团队已证实性激素能够通过蛋白RANKL及其受体RANK触发乳腺癌产生(Nature, doi:10.1038/nature09387; doi:10.1038/news.2010.504),其中RANKL和RANK是骨代谢中的关键因子。RANKL和RANK也因提供信号告诉乳腺细胞生长而将性激素与这些细胞关联在一起。正常情形下,这会在每个女性的怀孕和月经期间发生。然而,如果失去调节的话,乳腺细胞开始分裂和增殖,而且不会在它们应当死亡时死掉,这最终会导致乳腺癌产生(盘点:2014年Nature 杂志亮点研究成果)。
如今,在一项新的研究中,来自奥地利、美国、加拿大、西班牙和英国的研究人员发现RANKL也是BRCA1突变驱动的乳腺癌的主要驱动因子。在这项新的研究中,来自Penninger研究团队的研究生Verena Sigl证实在BRCA1发生突变的小鼠体内阻断RANKL/RANK系统导致大体上正常的乳腺,然而,在对照小鼠体内,浸润性乳腺癌产生了。相关研究结果于2016年5月31日在线发表在Cell Research期刊上,论文标题为“RANKL/RANK control Brca1 mutation-driven mammary tumors”。
为了确定这些结果对人类的重要性,研究人员从因BRCA1基因突变而已接受预防性乳房切除术的女性体内分离出乳腺组织细胞。在体外培养的人乳腺组织细胞中,抑制RANKL蛋白也会导致它们的生长和扩散能力显著下降。再者,研究人员研究了23,000多名女性,并证实RANK基因变异与携带BRCA1和BRCA2基因突变的女性有更高风险患上乳腺癌相关联。
Verena Sigl 解释道,“我们的发现也是激动人心的,这是因为已有被批准针对RANKL的药物狄诺塞麦(Denosumab)。它是一种抗体药物,具有非常少的副作用。它紧密地结合到RANKL上,因而抑制RANKL发挥作用。基于我们的发现,这种已被批准的药物狄诺塞麦或者未来将被批准的阻断RANKL/RANK的药物可能被用来预防BRCA基因突变携带者患上乳腺癌。”(Lancet:狄诺塞麦可以减少乳腺癌使用芳香酶抑制剂骨折的风险)
来自美国马里兰大学医学院的科学家已在小鼠体内试验过一种RANKL阻断药物以便预防乳腺癌。携带BRCA1突变的小鼠被分成两组。在对照组小鼠(作为第一组小鼠)中,多种早期的乳腺癌病灶形成。而在接受预防性RANKL阻断治疗的第二组小鼠中,在更长的观察时间内在它们的乳腺组织中几乎没有观察到恶性病变。
如今还需开展III期临床试验在人体内验证这种方法的疗效。若经验证有疗效的话,那么任何经测试发生BRCA1突变的女性可能需要服用RANKL阻断药物作为一种防御策略降低她因BRCA1突变而显著增加的乳腺癌风险。Josef Penninger补充道,“这项研究是很多科学家们开展国际合作的一个好例子,这种合作的宏伟目标是预防乳腺癌。癌症预防是我们如今在医学上面临的众多关键问题之一。我们也证实RANKL/RANK在性激素驱动的乳腺癌中发挥着关键性作用。如果揭示的这种机制确实在预防高危患者患上乳腺癌中有效的话,那么这可能能够被用来预防乳腺癌。如今,预防乳腺癌的一扇门已被打开,这能够非常快地开展测试。”
原始出处:
Sigl V, Owusu-Boaitey K, Joshi PA, Kavirayani A, Wirnsberger G, Novatchkova M, Kozieradzki I, Schramek D, Edokobi N, Hersl J, Sampson A, Odai-Afotey A, Lazaro C, Gonzalez-Suarez E, Pujana MA, Cimba F, Heyn H, Vidal E, Cruickshank J, Berman H, Sarao R, Ticevic M, Uribesalgo I, Tortola L, Rao S, Tan Y, Pfeiler G, Lee EY, Bago-Horvath Z, Kenner L, Popper H, Singer C, Khokha R, Jones LP, Penninger JM. RANKL/RANK control Brca1 mutation-driven mammary tumors. Cell Res. 2016 May 31. doi: 10.1038/cr.2016.69
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#抑制剂#
60
#CEL#
60
#Cell#
48
#RANKL#
70
不错的文章,多学习
156
不错的文章,多学习
114
学习了,不知监测方便不
124
57土豆块
136