NEJM:冠状窦缩小装置可使难治性心绞痛患者获益
2015-02-10 高晓方 译 医学论坛网
欧洲一项研究表明,在不适宜行血运重建的难治性心绞痛患者中,置入冠状窦缩小装置与其症状和生活质量显著改善具有相关性。论文发表于《新英格兰医学杂志》[N Engl J Med 2015, 372(6):519]。 冠状窦缩小装置 此项研究共纳入104例加拿大血管学会(CCS)分级为III或IV级的心绞痛(级别越高,因心绞痛而进行体力活动限制程度更大)和心肌缺血患者,不适宜行血运
欧洲一项研究表明,在不适宜行血运重建的难治性心绞痛患者中,置入冠状窦缩小装置与其症状和生活质量显著改善具有相关性。论文发表于《新英格兰医学杂志》[N Engl J Med 2015, 372(6):519]。

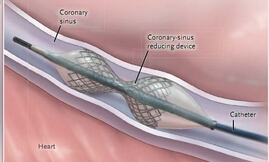
冠状窦缩小装置
此项研究共纳入104例加拿大血管学会(CCS)分级为III或IV级的心绞痛(级别越高,因心绞痛而进行体力活动限制程度更大)和心肌缺血患者,不适宜行血运重建并随机给予冠状窦缩小装置(治疗组)或假手术(对照组)。患者均不适宜接受血运重建。冠状窦缩小装置为可将血流重新分配至缺血心肌的球囊扩张、不锈钢、沙漏型器械。主要终点为6个月时CCS心绞痛分类至少改善两级的患者比率。
结果显示,6个月时,治疗组和对照组分别有35%和15%的患者CCS心绞痛分级至少改善两级(P=0.02)。治疗组有71%的患者CCS心绞痛分级至少改善一级,对照组则为42%(P=0.003)。

CCS分级变化
治疗组患者的生活质量较对照组显著改善(17.6对7.6;P=0.03)。两组患者在锻炼时间和壁运动指数平均变化改善方面无显著差异。6个月时,治疗组1例患者出现心梗;对照组1例患者死亡,3例出现心梗。
原始出处:
Verheye S1, Jolicœur EM, Behan MW, Pettersson T, Sainsbury P, Hill J, Vrolix M, Agostoni P, Engstrom T, Labinaz M, de Silva R, Schwartz M, Meyten N, Uren NG, Doucet S, Tanguay JF, Lindsay S, Henry TD, White CJ, Edelman ER, Banai S.Efficacy of a device to narrow the coronary sinus in refractory angina.N Engl J Med. 2015 Feb 5;372(6):519-27. doi: 10.1056/NEJMoa1402556.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







已阅
97
以阅
94
恩恩
97
明白
77
#难治性#
45