Nat Commun:METTL3通过m6A修饰介导APC的表达促进肿瘤的发生发展
2021-06-24 xiaozeng MedSci原创
结肠腺癌抑制基因(adenomatous polyposis coli,APC)被认为是一种关键的肿瘤抑制基因,其在抑制经典Wnt信号通路中起着至关重要的作用
结肠腺癌抑制基因(adenomatous polyposis coli,APC)被认为是一种关键的肿瘤抑制基因,其在抑制经典Wnt信号通路中起着至关重要的作用,而该通路主要调控细胞的增殖和分化。
既往研究显示,APC的功能丧失会导致β-catenin的异常稳定。反式激活的 β-catenin能够与TCF/LEF形成复合物,并激活许多重要的下游基因,如CCND1和MYC,最终促进肿瘤的发生发展。
在结直肠癌中APC的突变率可达80%。相比之下,APC在如食道鳞状细胞癌(ESCC)在内的其他类型癌症中却很少发生突变。然而,目前并不清楚APC的表达水平是否受表观转录组水平的调控,以促进肿瘤的发生发展。
METTL3的表达上调与ESCC患者的低生存率相关
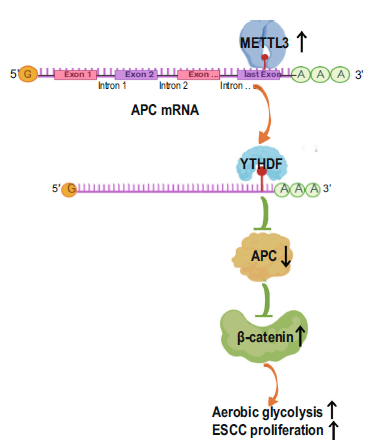
在该研究中,研究人员通过分析TCGA数据并分析200对ESCC标本及其邻近的正常组织,鉴定了METTL3(甲基转移酶样蛋白3)在肿瘤组织中高表达。m6A-RNA免疫沉淀实验发现,METTL3能够上调APC的m6A修饰水平,并招募YTHDF降解APC的mRNA。
METTL3促进ESCC发生发展的机制示意图
研究人员发现,降低APC的表达水平会上调β-catenin以及β-catenin介导的cyclin D1、c-Myc和PKM2的表达,进而增强有氧糖酵解作用、ESCC细胞的增殖和肿瘤的形成。此外,APC的表达水平下调与ESCC样本中METTL3的表达上调以及ESCC患者的不良预后相关。
总而言之,该研究结果揭示,METTL3/YTHDF介导的APC表观转录水平的下调能够通过上调Wnt/β-catenin通路,促进ESCC的发生发展。
原始出处:
Wang, W., Shao, F., Yang, X. et al. METTL3 promotes tumour development by decreasing APC expression mediated by APC mRNA N6-methyladenosine-dependent YTHDF binding. Nat Commun 12, 3803 (21 June 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#m6A#
64
#COMMUN#
55
#发生发展#
80
#MET#
65
#Nat#
55
#Mettl3#
78
结肠腺癌抑制基因(adenomatous polyposis coli,APC)被认为是一种关键的肿瘤抑制基因,其在抑制经典Wnt信号通路中起着至关重要的作用。
88
学习了
97
#APC#
53
#修饰#
97