Blood:创新药物MIR17PTi,miR-17-92前体抑制剂,在多发性骨髓瘤中的应用
2018-07-13 MedSci MedSci原创
MicroRNA-17-92(MiR-17-92)具有致癌性,是c-MYC(MYC)驱动的恶性肿瘤的一个极具潜力的治疗靶点。Eugenio Morelli等人开发了一种新型LNA gaomeR反义寡核苷酸(ASOs),来诱导RNase H介导降解MIR17HG初级转录本,进而抑制miR-17-92s的生成。主要的LNA-ASO(MIR17PTi)可通过靶向反义活性抑制48种实体瘤和血液瘤的癌细胞系
主要的LNA-ASO(MIR17PTi)可通过靶向反义活性抑制48种实体瘤和血液瘤的癌细胞系增殖,相比miR-17-92s抑制剂效果更显著。
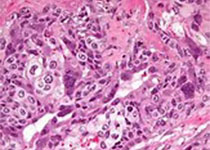
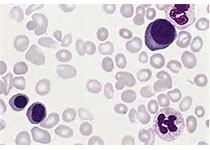
进一步针对多发性骨髓瘤(MM)进行研究时发现MIR17PTi可通过破坏患者来源的MM细胞的自我平衡的MYC/miR-17-92正反馈环(FFLs)来触发细胞凋亡,并诱导MYC依赖性的合成性致死。
此外,研究人员还发现在MM细胞中,以BIM为中心的FFL发生改变有助于MIR17TPi诱导细胞毒性。MIR17PTi在MM的临床相关小鼠模型(NOD-SCID小鼠)中表现出较强的抗肿瘤活性,并在非人类的灵长类动物中具有有利的安全性和药代动力学特征。
总而言之,MIR17PTi是一种新型药物,动物学实验已证实其具有抗肿瘤活性,需进一步开展临床试验评估其用于MM和其他MYC驱动的恶性肿瘤的疗效和安全性。
原始出处:
Eugenio Morelli, et al. Therapeutic vulnerability of multiple myeloma to MIR17PTi, a first-in-class inhibitor of pri-mir-17-92. Blood 2018 :blood-2018-03-836601; doi: https://doi.org/10.1182/blood-2018-03-836601
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#miR-17-92#
70
#多发性#
55
#miR#
64
#抑制剂#
56
#新药物#
71
学习学习谢谢
76
#创新#
61