Stroke:治疗不明原因栓塞性中风,阿司匹林与利伐沙班疗效相似,且更安全
2019-08-21 朱柳媛 中国循环杂志
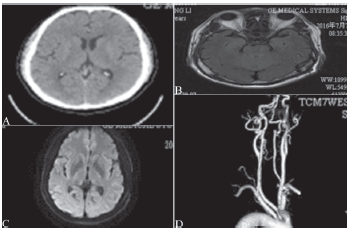
近日,Stroke杂志发表的NAVIGATE ESUS研究最新结果表明,对于存在颈动脉斑块或狭窄的不明原因栓塞性中风患者来说,阿司匹林(100 mg/d)和利伐沙班(15 mg/d)在预防中风复发方面疗效相似,但阿司匹林更安全。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好
111
谢谢梅斯提供这么好的信息,学到很多
73
中风是俗称,应该称为缺血性卒中吧
91
学习了,谢谢分享
94