卵巢畸胎瘤超声鉴别诊断
2020-08-18 即时超声 即时超声
卵巢畸胎瘤是卵巢生殖细胞肿瘤中最常见的良性肿瘤,卵巢囊性畸胎瘤又称成熟性囊性畸胎瘤,是常见的畸胎瘤类型。卵巢畸胎瘤的内容物可由2-3个胚层的组织形成,含有皮肤及其附件、毛发、牙齿、神经、脂肪、骨骼等。
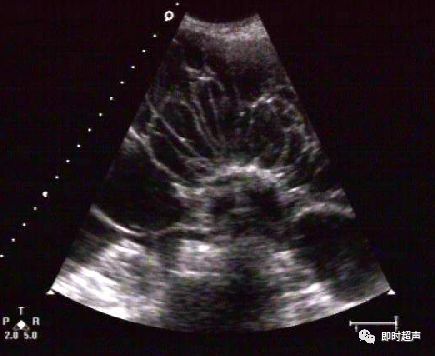
卵巢畸胎瘤是卵巢生殖细胞肿瘤中最常见的良性肿瘤,卵巢囊性畸胎瘤又称成熟性囊性畸胎瘤,是常见的畸胎瘤类型。卵巢畸胎瘤的内容物可由2-3个胚层的组织形成,含有皮肤及其附件、毛发、牙齿、神经、脂肪、骨骼等。 卵巢良性囊性肿瘤:特点:大多为囊性,囊壁光滑而薄,囊内膈均匀光滑,囊内壁突出规则乳头,囊壁及膈的血流不丰富,PI、RI值高。 粘液性囊腺瘤(mucinous cystadenoma):占卵巢所有肿瘤20%,恶变率5%,绝大多数单侧,瘤体较大,破裂可造成肿瘤的广泛种植。图象特点:以膈为主,从少量膈到极多量膈,呈多房性,囊壁及膈光滑,液体浑浊,后壁增强效应。10%可见乳头称粘液性乳头状囊腺瘤。 浆液性囊腺瘤(serous cystadenoma):为最常见的卵巢肿瘤,占卵巢肿瘤的27%。大部分为良性,但有较高的恶性变倾向,约有45%-50%可变为恶性。常为单侧性。图象特点:多为单房、壁薄、光滑、边界清,内部回声少,内有光带分隔为多房性,后壁回声增强。囊肿内壁显示有乳头状实质光团则为乳头状浆液性囊腺瘤。 卵巢成熟囊性畸胎瘤(mature teratoma):常见,声像图表现多种多样。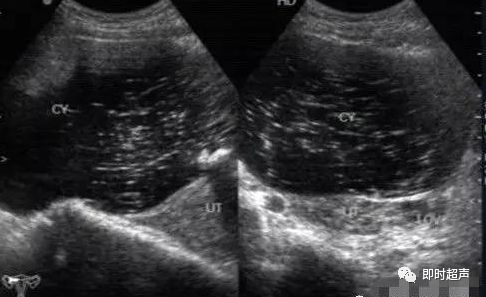


卵巢纤维瘤(fibroma):包膜不清的实性肿瘤,回声较衰减致密,可出现钙化斑。合并胸、腹水时则称为麦格氏综合症。

卵巢转移肿瘤——库肯勃格氏瘤(Krukenberg tumor):占转移肿瘤的80%。常为双侧实性肿瘤,回声衰减或反光较强,常见退行囊,大小不等。
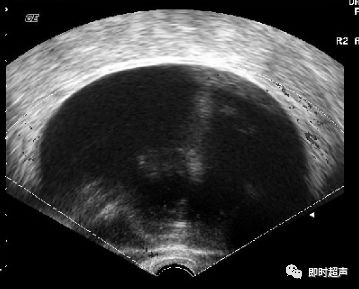
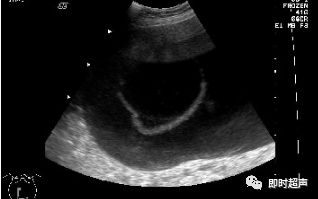
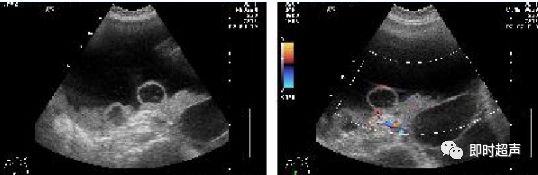
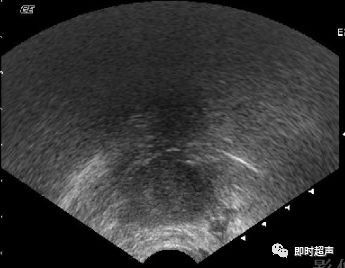
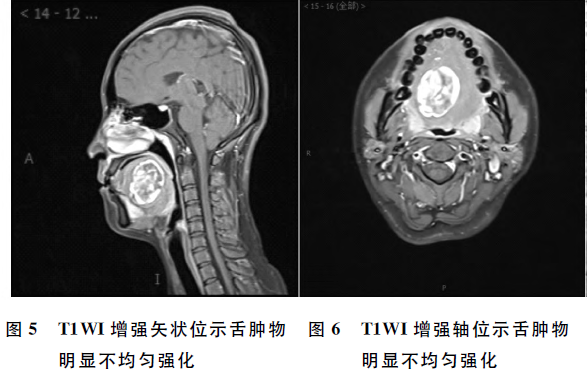
卵巢畸胎瘤声像图,因其构成成分及比例不同而表现不一,可表现为“脂液分层征”、“面团征”、“瀑布征”、“雪花征”、“线条征”、“壁上结节征”、“杂乱结构征”7种特异性声像图。
具有典型声像图的畸胎瘤较易诊断,造成误诊或漏诊者主要发生在单一组织构成的畸胎瘤,这类畸胎瘤发生率低,且超声表现与常见的由多种组织结构构成的畸胎瘤超声特点不同。因此需与卵巢子宫内膜异位囊肿、浆液性囊腺瘤、单纯性囊肿等相鉴别。
卵巢子宫内膜异位囊肿的超声表现为囊内密集点状回声,但其内也可出现带状间隔及团块状稍高回声,其与周围组织可粘连,囊壁厚而毛糙,较高回声较多沉积在中后部,呈絮状,较松散,加压探头或随访可见形态改变。患者一般有痛经病史。卵巢畸胎瘤的细密点状比内膜异位囊肿点状更细、更密、更高,团块状高回声亦更致密、更均匀、更高,且具清晰边界并常伴声影。易与囊样型和混合型卵巢畸胎瘤混淆,同时需要警惕两者并存的情况。

浆液性囊腺瘤:单房或多房囊腺瘤边界清晰,囊壁薄而完整,内壁光滑,纤细分隔光滑均匀。乳突状囊腺瘤在囊内壁上突起乳头,其囊壁、囊内间隔及乳突上可见细条状血流。
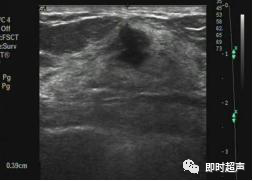
单纯性囊肿:卵泡囊肿、黄体囊肿、附件炎性囊肿、卵巢冠囊肿、阔韧带囊肿等,可通称为单纯性囊肿。一般内部透声好,无明显光点,超声表现为宫旁附件区囊性肿物,壁薄,内无回声。而卵巢畸胎瘤表现为单房状瘤内无回声时,可见囊壁局限性增厚,伴回声增强。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习
122
还送
129
👍🏻
131
#鉴别诊断#
84
👍
0