JNS:LSC分类与后纵韧带损伤、神经功能损伤及治疗选择无关
2012-08-23 紫川秀第二 丁香园
LSC(load sharing classification载荷分担分类标准是胸腰椎爆裂性骨折的载荷分担的分类系统,最初于1994年由Thoma McCormack等人提出,并发表在spine杂志上。当时提出该分类标准时是基于胸腰椎爆裂性骨折病人中有部分病人进行短节段固定时容易出现钉棒的断裂。Thoma等人对这类爆裂性骨折的病人进行了CT影像学表现的总结,提
LSC(load sharing classification载荷分担分类标准是胸腰椎爆裂性骨折的载荷分担的分类系统,最初于1994年由Thoma McCormack等人提出,并发表在spine杂志上。当时提出该分类标准时是基于胸腰椎爆裂性骨折病人中有部分病人进行短节段固定时容易出现钉棒的断裂。Thoma等人对这类爆裂性骨折的病人进行了CT影像学表现的总结,提出三个指标:1.受伤节段骨折椎体的爆裂程度;2.骨折爆裂碎片在受伤节段的位置;3.爆裂节段脊柱椎体的成角程度,具体的评分详见图1。
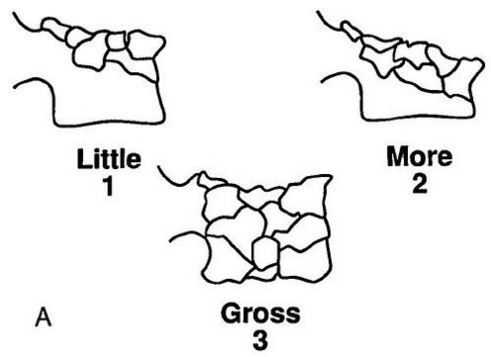
图1:A:骨折椎体的粉碎程度:轻<30%,1分;中30%-60%,2分;重>60%,3分。
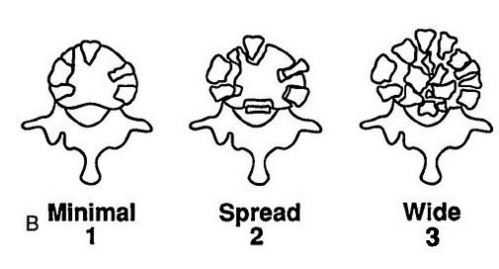
B:骨折块碎裂的位置:轴位CT上轻度移位<2mm,1分;移位>2mm,但不超过椎体横截面积的50%,2分;
移位>2mm,并且超过椎体横截面积的50%,3分。
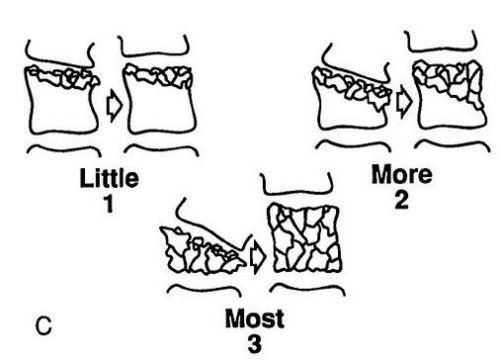
C:爆裂节段脊柱椎体的成角程度:纠正后成角≤3度,1分;纠正后成角4-9度,2分;纠正后成角≥10度,3分。
LSC最初设计时是用来评估术后短节段固定的患者是否会出现钉棒断裂以决定手术治疗的方式。一般认为LSC评分≥6分者行短节段固定容易出现内固定失败。但脊柱外伤后是否需要手术治疗还取决于其他各种因素,如患者的脊柱后纵韧带是否完整,脊髓是否损伤等,LSC并没有将上述指标包括在内。但胸腰椎爆裂性骨折的病人LSC和后纵韧带损伤,脊髓神经功能损伤及手术治疗方式等之间的关系尚不明确,来自美国费城的学者就上述问题进行了回顾性研究,研究结论发表在近期的Neurosurgery spine上。
研究者选取2006-2009年间在研究者所在机构就诊的胸腰椎爆裂性骨折的病人共44例(表1)。所有入选病人的暴力节段在T10-L2之间,屈曲牵张性损伤,感染,病理性骨折等椎体骨折除外。对所有患者进行CT的扫描和矢状位的重建,以便计算LSC评分;而对所有的患者进行MRI的检查,以便了解患者的后纵韧带,椎间盘,脊间韧带,脊上韧带,黄韧带等情况,后纵韧带损伤的评分分级:0分完整,2分不确定,3分破裂;使用ASIA及Frankle评分对患者的神经功能进行评估。参与LSC评分,MRI评分及神经功能评分的4位脊柱外科医生并不参与患者的手术治疗。
表1:患者的人口统计学数据

表2:LSS评分分布
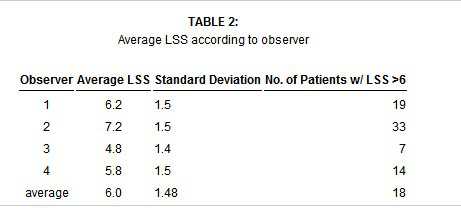
结果显示,LSS评分总分如表2所示,平均评分6.0±1.48,在四位观察者的统计中共有1位患者的平均LSS评分>6分。观察者的组间一致性:所有44位病人中,15位患者取得一致的治疗意见,其中4位患者LSS评分>6分,需要手术治疗;11位患者LSS评分<6分,进行保守治疗。平均Cohen Kappa=0.43分,有中度的一致性,而对LSS>6分的Kappa=0.24,只有较小的一致性(表3)。而LSS评分和治疗的选择,ASIA评分,Frankle分级,PLC损伤等相关性如表4所示。
表3:观察者的组间一致性
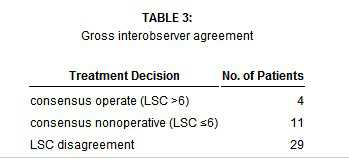
表4:LSS评分和治疗的选择,ASIA评分,Frankle分级,PLC损伤等相关性
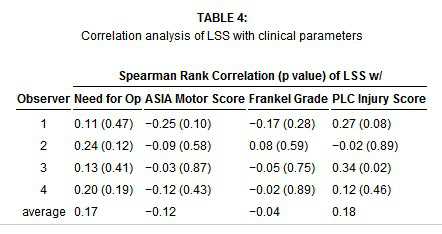
该研究结果表明,LSS评分和PLC损伤,脊髓神经功能状态,临床治疗方式选择没有直接的相互关系。所以将LSS评分作为一个手术指征是不恰当的。作者建议在患者进行手术或保守治疗的选择上应该引入无利益问题的第三方。
原文链接:
Radcliff K, Kepler CK, Rubin TA, Maaieh M, Hilibrand AS, Harrop J, Rihn JA, Albert TJ, Vaccaro AR. Does the load-sharing classification predict ligamentous injury, neurological injury, and the need for surgery in patients with thoracolumbar burst fractures?: Clinical article.J Neurosurg Spine. 2012 Jun;16(6):534-8. Epub 2012 Apr 6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#LSC#
61
#治疗选择#
74
#后纵韧带#
76
#损伤#
45
#神经功能#
57
#韧带#
63