Cell Death Dis:活性氧(ROS)的损伤与保护的博弈决定心肌缺血/再灌注的命运
2014-06-26 MedSci MedSci原创
6月19日,自然出版集团子刊Cell Death and Disease在线发表了健康科学研究所杨黄恬研究组题为 “Concentration-dependent wrestling between detrimental and protective effects of H2O2 during myocardial ischemia/reperfusion” 的最新研究成果,揭示了H
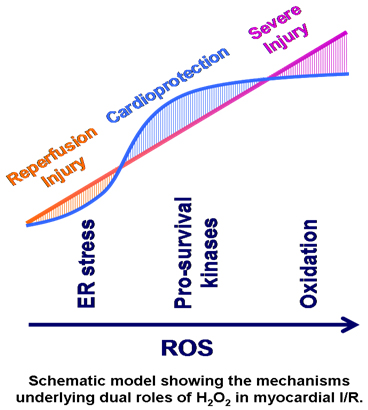
心肌梗塞后及时恢复缺血区的血供(再灌注)是挽救缺血心肌的必需步骤,但该过程伴随着严重再灌注损伤的发生。再灌注初期活性氧(reactive oxygen species, ROS)的大量释放被认为是造成这一损伤的主要因素之一。然而,ROS也作为启动者介导了缺血预处理(ischemic preconditioning, IPC)和后处理(ischemic postcondition, IPoC)等措施对抗心肌I/R损伤的保护作用。为了解释ROS 这种相互矛盾的双重作用,研究者提出了一种假设,即低浓度ROS 作为第二信使参与了心肌保护作用,而高浓度ROS 则导致细胞损伤,但如何界定ROS 起损伤或保护作用浓度界限目前尚无明确的研究,而且该理论无法完美解释众多应用抗氧化剂的临床实验没有显著心肌保护作用的事实。
博士研究生王志华、刘金龙等在杨黄恬研究员的指导下发现H2O2PC和PoC在10-100 mmol/L浓度依赖地激活RISK信号通路、抑制其下游的糖原合成酶激酶(glycogen synthase kinase, GSK)3-b活性,进而改善I/R后心功能;而低浓度(1-3 mmol/L)及高浓度(1 mmol/Lol/L) H2O2他则通过不同的机制加重了I/R后心功能不全。低浓度H2O2PC和PoC (1-3 mmol/L) 通过进一步上调心肌I/R导致的ER stress加重了I/R后心肌损伤,该效应在3 mmol/L H2O2处理下达到平台期;而高浓度H2O2 (≧100 mmol/L) 则通过促进氧化应激反应加重I/R后心肌损伤。研究发现证明了浓度是决定ROS不同作用的重要因素之一,揭示了ROS导致心肌I/R损伤和保护作用的浓度 阈值和其内在机制,其最终表现是不同浓度ROS启动/激活的损伤与保护通路博弈的结果。研究发现还为解释ROS矛盾作用的机理提供了新的视角,并为开发基 于ROS的缺血性心脏病的治疗措施提供了新的实验证据。
此研究得到了国家自然科学基金委和国家科技部973项目的资助。
原始出处:
Wang ZH, Liu JL, Wu L, Yu Z, Yang HT.Concentration-dependent wrestling between detrimental and protective effects of H2O2 during myocardial ischemia/reperfusion.Cell Death Dis. 2014 Jun 19;5:e1297
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
71
#Cell#
96
困扰大家的问题终于露出了冰山一角,很好的研究。
241
#Dis#
80
#活性氧#
73
#ROS#
66
#损伤#
0
#Death#
62