蝴蝶振翅 “魔剪”CRISPR花落谁家再起波澜
2016-08-19 佚名 生物谷
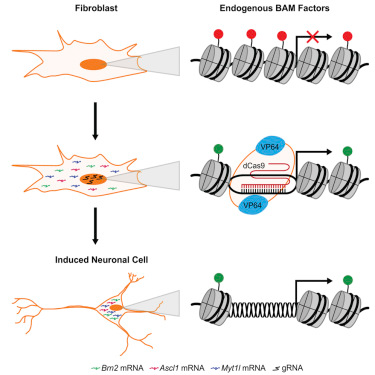
作为近年来生命科学领域最为激动人心的技术,CRISPR技术以令人难以置信的速度被业界所接受。科学家们认为这一技术未来将具有难以想象的使用价值。然而,在这一技术背后,还有一个激烈的专利战尚未解决。两位顶级的科学家——来自加州大学伯克利分校的Dr. Jennifer Doudna和来自MIT的张锋就该技术的专利权归属问题一直在进行角逐。 回到故事的开端,加州大学伯克利分校的生化学家Dr. Jen
作为近年来生命科学领域最为激动人心的技术,CRISPR技术以令人难以置信的速度被业界所接受。科学家们认为这一技术未来将具有难以想象的使用价值。然而,在这一技术背后,还有一个激烈的专利战尚未解决。两位顶级的科学家——来自加州大学伯克利分校的Dr. Jennifer Doudna和来自MIT的张锋就该技术的专利权归属问题一直在进行角逐。
回到故事的开端,加州大学伯克利分校的生化学家Dr. Jennifer Doudna于2012年5月份提交了关于CRISPR技术的专利申请,而张锋则于2013年提交了一份相似专利,不过他同时要求就该专利进行快速审批待遇,并最终于2014年4月份获得了专利授权。
两名科学家同时宣称自己发明了这一技术,并于今年一月份对簿公堂。然而,本周爆出的一份来自一名研究人员的邮件却让这一事件再次被推上风口浪尖。该研究人员曾经在张锋所在的实验室工作,在他给Doudna的邮件中称,MIT-哈佛方面误导了专利局。该邮件是于去年二月份发出的,最近被美国专利局所公开。据称,这名工作人员曾经于2011年在张锋的实验室独立进行CRISPR相关方面的工作,在最初的专利申请版本中,这名工作人员的名字也位列发明者之列。2012年这名工作人员返回中国,当时Doudna的论文刚刚发表,他指责张锋迅速进入该领域并没有告知他。在那段时间,这名工作人员将项目失败的相关数据都展示给了实验室感兴趣的研究人员。
不过,有意思的是,这封邮件的主题实际上是一封发给Doudna的工作申请。他在原文中称,我们(张锋实验室)在看到你的论文之前并未找到如何有效利用CRISPR的方法,因此我认为这种革命性的方法不能被错误的授权。据了解,目前这名研究人员在加州大学旧金山分校从事博士后工作且并未对此进行评价。
不过,来自张锋所工作的MIT-哈佛Broad中心的Lee McGuire在声明中表示,首先该邮件的作者当时仅是一个轮转的博士研究生,并证实他在2011年10月-2012年6月在张锋实验室从事CRISPR的相关工作。但是他表示,从张锋和其学生的一系列邮件中,就已经证明这封邮件内容的错误。例如2011年8月,张锋向其介绍了Cas9在基因编辑方面相关方面信息;2011年10月他向其解释tracrRNA在crRNA二聚体装载在Cas9过程中的重要性等;2011年11月,他承认由于未能完全遵循张锋等人设计的试验计划操作而导致了部分实验的失败。事实上,这都暗示了他是在张锋的指导下进行研究的。
抛开上述争论。或许有人会好奇,为何这一技术会受到大家的广泛关注以及两方面的激烈争论?这主要是因为这一技术代表着未来一个极具前景的市场。尽管这一技术目前仅处于临床前研究阶段,但是今年美国和中国都将开展利用该技术治疗癌症的临床研究,预计2017年将会有更多的临床研究启动。众多医药巨头、学术机构都寻求首先启动临床研究并率先获得FDA的上市批准。一旦该技术成为现实,将会为所有人带来数以十亿计美元的收益。目前,在这一领域的公司包括张锋创立的Editas、CRISPR Theraeutics、Caribou Biosciences、Intellia以及诺华公司等。
生物谷小编认为,这一技术毫无疑问是具有划时代意义的,但是希望这一技术的专利之争仅止于学术争论,不要影响到产业利用CRISPR技术治疗疾病研究的进程。毕竟当科学争论变成了肥皂剧,那么就失去了科学的庄严性。
原始出处:
CRISPR patent battle heats up as new email disputes Zhang’s claims
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#魔剪#
74
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
106
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
96
阅读了。
107
写的很好的!!
86
#CRISPR#
62
阅读了。
86
值得学习
45
值得学习
54
好好学习一下
46