查出颈动脉斑块需要吃他汀和阿司匹林治疗吗?
2019-06-21 郭艺芳 郭艺芳心前沿
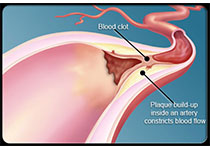
近年来颈动脉超声检查普遍开展,很多患者或健康查体者被发现有颈动脉斑块。存在颈动脉斑块者需要应用他汀和阿司匹林治疗吗?这是临床上经常被患者问到的问题。
若颈动脉斑块导致了颈动脉明显狭窄(狭窄≥50%),其处理原则与确诊冠心病或缺血性卒中相同(均属于动脉粥样硬化性心血管疾病),应该立即接受他汀治疗,将LDL-C控制在1.8mmol/L以下。若无禁忌证,还应接受阿司匹林抗血小板治疗。这两类药物均需长期服用。
若颈动脉斑块未导致明显狭窄(狭窄程度<50%),则需要评估患者是否存在心血管病或其他心血管病危险因素,决定是否应用他汀治疗。可有以下几种情况:
1、已确诊冠心病或缺血性卒中,无论颈动脉有无明显狭窄均应立即接受他汀治疗,将LDL-C控制在1.8mmol/L以下;
3、年龄≥40岁的糖尿病患者,且LDL-C>2.6 mmol/L,需要接受他汀治疗;
4、慢性肾病(III期或IV期)且LDL-C>2.6 mmol/L,需要接受他汀治疗;
5、存在高血压或其他危险因素、且LDL-C>3.4 mmol/L,建议积极改变不良生活习惯,特别是控制饮食并增加运动、戒烟限酒,将LDL-C降至<3.4 mmol/L。必要时也可应用他汀治疗。
以上是一种简单的判定方法,在临床上还应全面分析患者其他情况综合判断。
若颈动脉斑块未导致明显狭窄(狭窄程度<50%),是否应用阿司匹林治疗也需全面考量。如果患者合并冠心病或缺血性卒中,应该应用阿司匹林治疗。
年龄50-70岁之间的患者,如果颈动脉斑块未导致明显狭窄,并且患者未合并冠心病或缺血性卒中等动脉粥样硬化性心血管疾病,需要进行谨慎评估后决定是否应用阿司匹林。如果同时存在高血压、糖尿病、吸烟、高血脂等多种危险因素,并且没有出血的高危因素,可以考虑应用小剂量阿司匹林治疗。
年龄<50岁或者>70岁,发现颈动脉斑块但未导致明显狭窄,并且没有合并冠心病或缺血性卒中,一般无需应用阿司匹林。
关键信息:没有导致明显狭窄的颈动脉斑块不是应用他汀和阿司匹林治疗的指征。有人一见到斑块就应用他汀和阿司匹林,这是不合理的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#颈动脉#
102
#颈动脉斑块#
61
#斑块#
68
学习了谢谢分享
116