Cancer:结婚益处多多 可改善癌症生存率且帮助延年益寿
2016-04-13 佚名 生物谷
一项刊登在国际杂志Cancer上的研究论文中,来自加州癌症预防学会的研究人员表示,结婚戒指或许是抵御癌症的强大药物,研究者在文章中指出,对于癌症而言,已婚人士似乎拥有显著的生存优势,相比已经结婚的男性患者而言,单身的男性癌症患者的死亡率要高于前者27%,而单身女性癌症患者的死亡率要高于已婚女性死亡率的19%。 文章作者Scarlett Li

图片来源:medicalxpress.com
-一项刊登在国际杂志Cancer上的研究论文中,来自加州癌症预防学会的研究人员表示,结婚戒指或许是抵御癌症的强大药物,研究者在文章中指出,对于癌症而言,已婚人士似乎拥有显著的生存优势,相比已经结婚的男性患者而言,单身的男性癌症患者的死亡率要高于前者27%,而单身女性癌症患者的死亡率要高于已婚女性死亡率的19%。
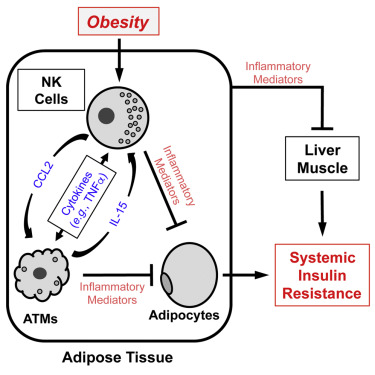
文章作者Scarlett Lin Gomez说道,我们发现的这种效应非常显著,过去10至15年的研究结果表明,婚姻对于癌症患者也存在类似的效应,而这种效应总是因为已婚人士的配偶给予的支持和关爱。但已婚个体更趋向于有较高的混合性收入和更好的保险体系,为此研究人员决定进一步研究来揭示是否金钱在已婚配偶的生存率上扮演着重要角色。
研究人员分析了来自加州80万名个体的健康记录,这些个体在2000至2009年间均被诊断出患有侵袭性的癌症,而且研究者对这些个体一直追踪观察到2012年;研究者表示,财力状况对个体击败癌症的机会并不具有一定影响,反而来自配偶的关怀和支持是癌症患者获益且提高生存率的关键,比如带着他/她去定期进行检查,给对方准备一顿营养的餐食,并且提醒对方按时服药等。
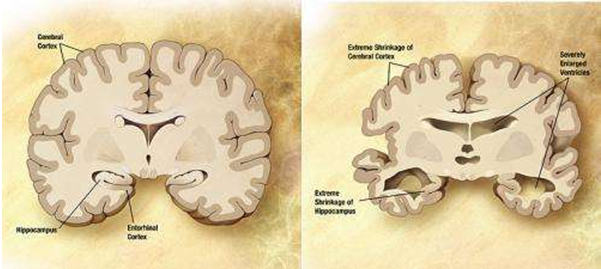
已婚的癌症患者往往会从情感上的支持获益,而这会减少患者的压力并且改善患者疾病进展的步伐;Gregory Masters博士说道,致力于护理事业的价值或许对于改善癌症病人的生存率非常有必要,本文研究结果或许并不是仅对于改善癌症患者的生存有效,我们都知道不论疾病困扰,当两个人结为伴侣共同生活扶持,他们或许也会变得比较长寿。
研究者表示,结婚对个体生存的有益影响或许在各种族人群中都表现不同,白人或许会因结婚获益较多,而西班牙裔的美国人和太平洋岛居民或许获益较少,而出生在美国的西班牙裔的美国人和太平洋岛居民相比出生在国外的个体而言获益的程度又会增加。
原始出处:
Scarlett Lin Gomez,et al.Effects of marital status and economic resources on survival after cancer: A population-based study.Cancer.11 APR 2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#癌症生存率#
81
#延年益寿#
61
结婚?发昏!
105
#生存率#
74
高大上的文章
133
值得学习
135
为婚姻有找到新的yan
222
癌症的生存率,也是临床医生努力的方向。
90