Eur Heart J:先天性心脏病成人生命最后一年:死亡原因和护理模式分析
2022-08-31 MedSci原创 MedSci原创
在CHD成年患者生命终结时,大量使用了可能可以避免的重症护理。这可能意味着针对CHD成年患者的临终关怀可以得到改善。
在过去的50年里,先天性心脏病(CHD)患者的预期寿命有了相当大的增长。例如,现在患有CHD的儿童有97%长大成人,而20年前这一比例为85%。尽管有这些改善,很大一部分成年CHD患者仍然有症状,并且具有过早死亡的高风险(死亡的中位年龄仍低于50岁)。长期后遗症,如心力衰竭和心律失常,随着患者年龄的增长越来越频繁,对生活质量和总生存期产生负面影响。为了了解成年CHD患者的死亡轨迹,需要进一步调查其生命的最后一年。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在(i)明确CHD患者的死亡原因,(ii)描述成年CHD患者生命最后一年的医疗资源使用模式。

这项回顾性死亡率随访研究使用了来自BELCODAC的医疗保健索赔和临床数据,其中包括来自比利时的CHD患者。医疗保健利用包括心血管手术、CHD专科就诊、全科医生就诊、住院、急诊(ED)就诊、入住重症监护病房(ICU)和专科姑息治疗,并使用代码进行识别。
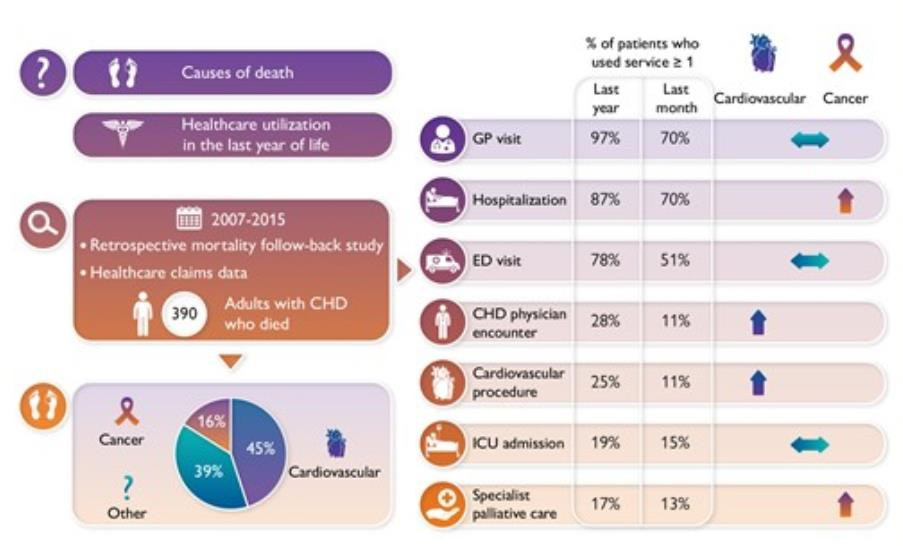
在纳入的390名患者中,几乎有一半(45%)的研究人群死于心血管疾病。在生命的最后一年,87%的患者住院,78%的患者去了急诊科,19%的患者住进了ICU。17%的患者接受了专科姑息治疗,而现定于因心血管原因死亡的患者时只有4%的患者接受了专科姑息治疗。
由此可见,在CHD成年患者生命终结时,大量使用了可能可以避免的重症护理。这可能意味着针对CHD成年患者的临终关怀可以得到改善。未来的研究应该根据病人的需求和偏好进一步研究临终关怀的提供方式,以及医疗系统如何充分响应CHD患者需求。
原始出处:
Liesbet Van Bulck,et al.Last year of life of adults with congenital heart diseases: causes of death and patterns of care.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac484/6676419
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#死亡原因#
0
#ART#
88
#先天性#
144
#HEART#
92