JACC:肺功能的下降会增加心血管疾病风险
2018-08-29 MedSci MedSci原创
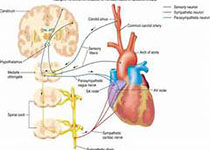
肺功能不全会增加心血管疾病(CVD)的发生风险。本研究的目的旨在评估肺功能的纵向下降是否与心衰、冠心病和卒中的发生相关。本研究纳入了ARIC 临床研究中的10351名无CVD的参与者,平均年龄为54 ± 6岁,女性占56%,白种人占81%。快速肺功能下降定义为1s用力呼气量(FEV1)或用力肺活量(FVC)下降的最大四分位数(n=2585)。经过平均17 ± 6年时间的随访,心衰的发生率为14%,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
64
#ACC#
54
#疾病风险#
54
#血管疾病#
59
学习了,谢谢作者分享!
91