BMC Endocr Disord:新诊断2型糖尿病患者高血压的昼夜节律与血管靶器官损害
2015-12-26 phylis 译 MedSci原创
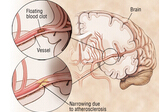
背景:与非糖尿病患者相比,2型糖尿病患者心血管疾病包括卒中的发生率较高。高血压患者血压晨峰(MBPS)与钝化收缩期日夜比(SNF)与心血管时间的发生相关。评估新诊断为糖尿病患者的MBPS或者糖尿病早期时间点的血管靶器官损伤的相关性尚未研究方法:对100例初诊为2型糖尿病的患者和100例年龄和性别相匹配的对照受试者进行动态血压监测。计算了MBPS和SND比率。早期血管靶器官损害的指标包括脉搏波传导速
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMC#
62
#新诊断#
74
#靶器官#
83
#器官损害#
71
#Disord#
57
不相关?
161
不相关?
79
额……
155
谢谢分享!
169
谢谢分享!
141