让肺结核无所遁形
2016-08-06 张章 中国科学报
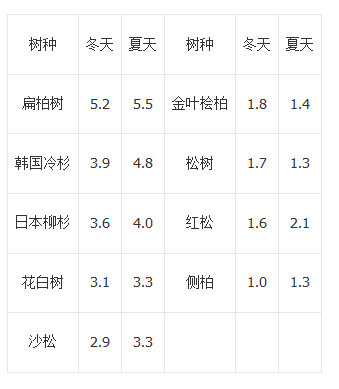
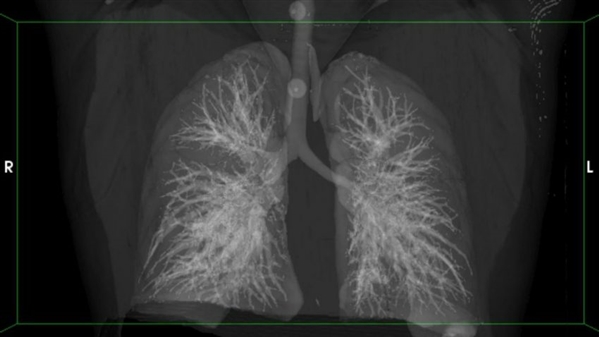
肺结核患者肺部扫描图像 图片来源:Hanif Esmail 高技术肺部成像有助于鉴别高风险肺结核潜在患者人群。在日前举行的第21届国际艾滋病大会上,出席肺结核特别讨论会的研究人员提出了鉴别能否治愈肺结核的新方法。这颠覆了人们认为肺结核隐藏于肺部并可能全面爆发的传统观念。 “活跃”肺结核每年约导致150万人死亡,但世界卫生组织(WHO)认为,全世界1/3的人口存在潜在的肺结核,这意味着结核杆菌

肺结核患者肺部扫描图像 图片来源:Hanif Esmail
高技术肺部成像有助于鉴别高风险肺结核潜在患者人群。在日前举行的第21届国际艾滋病大会上,出席肺结核特别讨论会的研究人员提出了鉴别能否治愈肺结核的新方法。这颠覆了人们认为肺结核隐藏于肺部并可能全面爆发的传统观念。
“活跃”肺结核每年约导致150万人死亡,但世界卫生组织(WHO)认为,全世界1/3的人口存在潜在的肺结核,这意味着结核杆菌不是在唾液中培养的,但如果混合这种细菌,人体免疫细胞仍会释放干扰素。因此,一种名为“迟发型超敏反应”的皮肤测试也被广泛用于确定潜在肺结核。
但在这些风险人群中,只有约10%的人在生命中的某一时刻会发展出肺结核。而且肺结核防控领域的一大挑战是无法甄别谁处于高风险中。潜在患者的肺部X射线结果也不能显示任何异常。此外,WHO还建议,在治疗感染了艾滋病病毒的潜在肺结核患者时,应使用抗结核药物异烟肼进行预防。但人们通常不采取该措施。
在新研究中,科学家使用更复杂的技术观察了35位南非艾滋病患者的肺部。标准测试结果显示,他们均有潜伏的肺结核。一组参与者使用计算机断层成像技术(CT)进行扫描,另一组则采用正电子放射断层造影术(PET)。CT显示的肺部解剖学细节远比X射线更详细,而PET则需注射放射性葡萄糖,通过观察代谢活跃细胞分辨结核杆菌的存在。
结果发现,10位参与者的肺部存在“热”节点。“我们看到了该疾病相当壮观的临床表现。”美国国家过敏症和传染病研究所肺结核研究主管Clifton Barry说。Barry在南非开普敦大学也拥有一个实验室。(Barry团队和Rob Wilkinson团队在开普敦大学进行了该研究。)但该小组在其他25人的肺部没有发现热点。
研究人员随后让每位参与者服用了异烟肼。在扫描和开始治疗后的几周,肺部有热点或异常CT扫描结果的10位患者中有4位出现了肺结核症状,而且其他两人唾液中也出现了结核杆菌。这些扫描结果揭示了哪些人会发展症状并急需全面肺结核治疗。全面肺结核治疗是指在6个月里服用3种不同的药物。
“这些数据令人叹服。”美国康奈尔大学结核病专家David Russell说,“从未有研究达到这样的清晰度。”
在治疗期间,研究人员继续进行了肺部扫描,他们观察到参与者的肺部异常逐渐消失,这意味着科学家能使用该技术分析治疗的有效性。“对很多人而言,这为弄清结核病是否需要治疗6个月开辟了新途径。”丹麦哥本哈根大学传染性疾病专家Jens Lundgren说,“如果我们能区分出那些能缩短疗程的患者,将有助于实现个体化用药。”由于标准治疗方案并不适用于所有患者,因此这将是一个突破。
Barry表示,这10位参与者身上的结核病距离“潜伏”也许还很远,其他25位参与者中的一些人并没有潜在的结核病。他怀疑,由于其免疫系统已经在过去某一时间清除了相关细菌,这些人体内只是出现了响应结核杆菌的干扰素伽马。“认为全世界1/3的人有潜伏的结核病是错误的。”Barry说,“这一数字虽然被广泛用于科学论文,但完全具有误导性。”
瑞士日内瓦非营利性组织“终止结核病伙伴”负责人Lucica Ditiu也认为,“潜伏”这一用词并不精确。“新研究数据非常有趣,我们应当进一步推进。”Ditiu说。
不幸的是,CT和PET扫描费用很高,Barry承认,让20多亿人进行检查不切实际,因为被定义为肺结核“潜伏”者的大部分人来自贫困国家。不过,他指出,扫描结果在研究中十分有用,例如在新结核药物早期测试中,扫描有助于大规模有效性研究的推进。
另外,Wilkinson还发现了鉴别具有活跃传染性患者的替代性方法。他进行了一种转录组分析,对比了上述10位肺部存在热点的参与者与其他25位参与者体内被开启的免疫基因。6个理论上能鉴别那些最有可能发展出症状并能传播该疾病的人的“生物学标记”浮出水面。另外,其他实验室近日也发现了这些转录生物学标记。
Barry认为,平均而言,感染了活性结核杆菌的每个人都能将病原体传播给10人中的其他人。“如果我们能在传染发生前,鉴别出临床症状不明显的患者,将对消灭结核病至关重要。”他说。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











不错哦继续关注
111
很好,不错,以后会多学习
105
很好,不错,以后会多学习
71
这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
89
好好学习一下
84
好好学习一下
64
#结核#
53