AANA:麻醉前可不可以来一颗PDE5抑制剂?
2016-03-24 zhaoshuang译 MedSci原创
近期美国麻醉护士学会(AANA)称,男性在术前一天不要使用治疗勃起功能障碍的药物!常见的包括伟哥和西力士。知道为什么术前不能吃,不做手术就能吃吗?因为一氧化氮!这些药物里含有能够舒张血管和松弛肌肉的一氧化氮,也是为什么血液可以充到小头里的原因。不过,这些药物在人体内的清除时间超过24小时。所以如果手术前吃了这些药,麻醉风险就会大大升高,麻醉时或使用其他药物时,可能出现血压的急剧下降。所以,男性在术
近期美国麻醉护士学会(AANA)称,男性在术前一天不要使用治疗勃起功能障碍的药物!常见的包括伟哥和西力士。
知道为什么术前不能吃,不做手术就能吃吗?
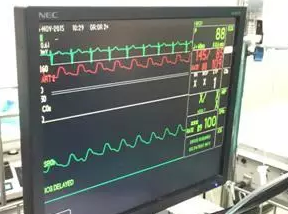
因为一氧化氮!这些药物里含有能够舒张血管和松弛肌肉的一氧化氮,也是为什么血液可以充到阴茎的原因。不过,这些药物在人体内的清除时间超过24小时。所以如果手术前吃了这些药,麻醉风险就会大大升高,麻醉时或使用其他药物时,可能出现血压的急剧下降。
所以,男性在术前和麻醉医师谈话的时候,要交代清楚药物使用情况,包括治疗勃起功能障碍的药物哟。可别嫌丢脸,生命不是儿戏。只有充分的了解之后,麻醉医师才能更好的制定麻醉计划,患者也才能处在更安全的环境中。
当然,治疗勃起功能障碍的药物只是一个例子,生活中患者正在服用的其他处方药或替代药物,也需要与医师进行充分的沟通。
原始出处:
Men, avoid impotence drugs before surger.MedicalXpress.March 21, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













不错哦,会学到很多
115
#ANA#
71
#PDE5抑制剂#
64
#抑制剂#
68
应该了解
159
应了解
146
确实在术前谈话有必要去了解
158
#AAN#
52