Nature Cell Biology:日美科学家发现造血干细胞持续造血机理
2017-03-20 佚名 科技部
日本九州大学研究生院与美国Albert Einstein医科大学的联合研究小组在世界上首次发现,间叶干细胞也可以根据遗传基因及蛋白质表达进行分类,而且它们还能形成各种细胞活素(维持干细胞造血功能的物质)。这一发现为弄清生命体内维持干细胞功能的复杂机制,打开了一个缺口, 有可能对研究形成高效增殖造血干细胞新方法,乃至加快再生医疗发展作出贡献。
初期的生命由一个干细胞发育而成。根据近年的研究,干细胞不仅存在于胎儿期,在成年人的各个脏器中,都存在着能够使该脏器再生的“脏器特异干细胞”。这些细胞具备终身无限增殖的能力,但通常情况下由于受到严格限制而多数处于“休眠状态”;在脏器受到损害等情况时,则根据需要发生增殖、分化。干细胞仅在特殊环境下“休眠”,这种环境被称作“龛”。
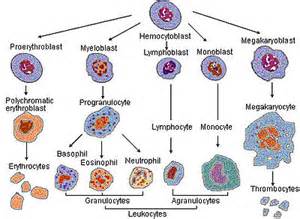
日本九州大学研究生院与美国Albert Einstein医科大学的联合研究小组在世界上首次发现,间叶干细胞也可以根据遗传基因及蛋白质表达进行分类,而且它们还能形成各种细胞活素(维持干细胞造血功能的物质)。这一发现为弄清生命体内维持干细胞功能的复杂机制,打开了一个缺口, 有可能对研究形成高效增殖造血干细胞新方法,乃至加快再生医疗发展作出贡献。
该成果发表在2017年2月20日的《Nature Cell Biology》电子版上。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Bio#
65
#CEL#
65
#Biol#
58
#科学家发现#
61
#Nat#
63
#Cell#
64
学习新知识谢谢分享
82
#造血干细胞#
66
#造血#
60
造血干细胞终生可以造血。
0