阜外医院李建军等在ATVB杂志发表研究,接受冠脉造影的患者中有3.5%为可能或明确家族性高胆固醇血症,但无一人LDL-C达标
2016-12-14 卢芳 中国循环杂志
近期中国医学科学院阜外医院李建军等在8000余例冠脉造影患者中进行的研究发现,有3.5%的患者具有明确(1%)和可能(2.5%)的家族性高胆固醇血症,但无一人低密度脂蛋白胆固醇(LDL-C)控制达标。 研究显示,在这8000余人中,女性患家族性高胆固醇血症为4.7%,远高于男性的2.9%。此外,不论男女,≤40岁以下者家族性高胆固醇血症更为多见,其中女性患病率为13.5%,男性患病率为9.3%(图
近期中国医学科学院阜外医院李建军等在8000余例冠脉造影患者中进行的研究发现,有3.5%的患者具有明确(1%)和可能(2.5%)的家族性高胆固醇血症,但无一人低密度脂蛋白胆固醇(LDL-C)控制达标。
研究显示,在这8000余人中,女性患家族性高胆固醇血症为4.7%,远高于男性的2.9%。此外,不论男女,≤40岁以下者家族性高胆固醇血症更为多见,其中女性患病率为13.5%,男性患病率为9.3%(图1)。
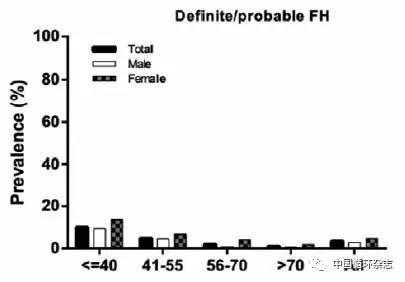
图1 不同年龄性别行冠脉造影患者中明确或可能的家族性高胆固醇血症流行情况
在明确和可能的家族性高胆固醇血症患者中,男性有82.7%为早发冠心病,女性仅为70.6%。“早发”冠心病的定义为男性<55岁,女性<60岁时发生冠心病。
研究者发现,虽然受试患者高胆固醇血症患病率不低,但无一例患者其LDL-C控制在<100 mg/dL。
研究显示,明确或可能的家族性高胆固醇血症患者中有20.6%未接受治疗;接受调脂治疗者中,接受低强度治疗者为6%,中等强度者为68.3%,高强度治疗者为5%。
研究者指出,这提示家族性高胆固醇血症患者的药物治疗,他汀类药物剂量以及治疗后反应都存在短板。而且很多患者被建议或开始接受治疗,时机较晚,并且已经罹患冠心病。
另外,在245例接受基因突变分析的明确和可能的家族性高胆固醇血症患者中,115例患者基因具有风险变异,检出率为46.9%。
其中,尤以低密度脂蛋白受体(LDLR)基因突变多见,而载脂蛋白B(APOB)基因次之,前蛋白转化酶枯草溶菌素9(PCSK9)基因殿后。基因突变阳性者其LDL-C水平更高。
研究者认为,该研究纳入的受试者来自全国各地,一定程度上可反映我国当前家族性高胆固醇血症的流行情况以及基因变异状况。
基于这项研究以及家族性高胆固醇血症的危害,研究者建议,有必要在血脂中心、冠心病中心等患者较为集中的医疗单元对前来就诊的患者开展家族性高胆固醇血症的筛查,以便患者尽早接受治疗。医院和心血管医生需要加强患者本人及其亲属对疾病的认识,以更有效控制疾病。
这项研究共纳入8050例行冠脉造影患者,其中家族性高胆固醇血症主要依据荷兰脂质诊所网络诊断标准,患者亲属主要依据查询患者及亲属本人提供的医疗记录。研究者还对患者LDLR、APOB和PCSK9等基因的外显子进行了测序。
原始出处:
Li JJ, Li S, Zhu CG, et al. Familial Hypercholesterolemia Phenotype in Chinese Patients Undergoing Coronary Angiography. Arterioscler Thromb Vasc Biol. ATVB AHA.2016 Dec 8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阜外医#
49
#TVB#
59
#阜外医院#
0
#高胆固醇血症#
53
#LDL#
53
#冠脉造影#
71
#造影#
53
#家族性#
53
学习了。。。
88