盘点:近年非霍奇金淋巴瘤研究进展汇总
2016-09-23 MedSci MedSci原创
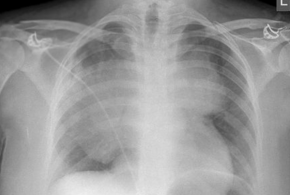
非霍奇金淋巴瘤(NHL)是一种始于淋巴细胞的肿瘤,是美国第六大最常见的癌症类型。发病原因尚不明确,但至今未发现其风险因素,如免疫系统抑制和暴露于某些感染。早期症状包括腋窝、颈部和腹股沟淋巴结肿大,伴有发热、胸痛、盗汗、体重减轻等。 在过去的30年里,NHL的发病率急剧上升。例如,在1990 - 2012年,以色列NHL的发病率上升了27%。目前研究人员尚不清楚发病率提高的原因,但它却
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很好的总结
93
学习收藏了
115
#研究进展#
55
有用的知识,谢谢分享
103
继续关注
102
谢谢分享!
87
继续关注!
55