BMJ:肺癌患者接受胸腔镜或开胸手术 其术后生存率相当
2014-10-20 高晓方 中国医学论坛报
一项英美联合研究表明,接受胸腔镜肺叶切除的肺癌患者在总体、癌症特异性和无病生存率方面均与接受开胸手术者相当。论文10月2日在线发表于《英国医学杂志》(BMJ)。 研究纳入2007-2009年间接受胸腔镜或开胸肺叶切除术的肺癌患者6008例,其中78%(n=4715)接受开胸手术,中位年龄74岁,中位随访时间40个月。 结果为,在各治疗组均为1195例患者的配对分析中,两组患者的3年
一项英美联合研究表明,接受胸腔镜肺叶切除的肺癌患者在总体、癌症特异性和无病生存率方面均与接受开胸手术者相当。论文10月2日在线发表于《英国医学杂志》(BMJ)。
研究纳入2007-2009年间接受胸腔镜或开胸肺叶切除术的肺癌患者6008例,其中78%(n=4715)接受开胸手术,中位年龄74岁,中位随访时间40个月。
结果为,在各治疗组均为1195例患者的配对分析中,两组患者的3年总体生存率(70.6%对68.1%,P=0.55)、无病生存率(86.2%对85.4%,P=0.46)和癌症特异性生存率(92%对89.5%,P=0.05)差异均无统计学显著性。
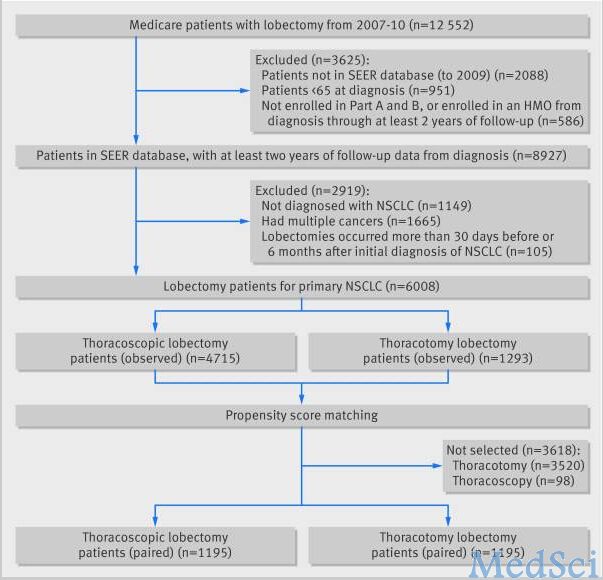
Fig 1 Patient selection flow chart. HMO=health maintenance organization; NSCLC=non-small cell lung cancer; SEER=Surveillance, Epidemiology and End Results
Patient selection flow chart. HMO=health maintenance organization; NSCLC=non-small cell lung cancer; SEER=Surveillance, Epidemiology and End Results
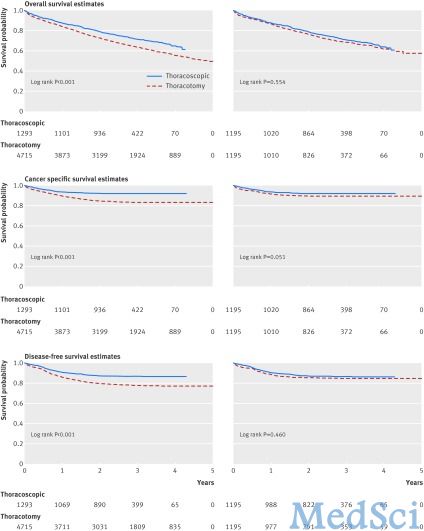
Fig 2 Kaplan-Meier survival plots (time until death with number of participants at risk) for thoracoscopic and thoracotomy lobectomy in unmatched (left side) and matched (right side) samples
Kaplan-Meier survival plots (time until death with number of participants at risk) for thoracoscopic and thoracotomy lobectomy in unmatched (left side) and matched (right side) samples
原始出处:
Paul S1, Isaacs AJ2, Treasure T3, Altorki NK4, Sedrakyan A5.Long term survival with thoracoscopic versus open lobectomy: propensity matched comparative analysis using SEER-Medicare database.BMJ. 2014 Oct 2;349:g5575. doi: 10.1136/bmj.g5575.[pdf free]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肺癌患者#
59
#BMJ#
65
#开胸手术#
64
#生存率相当#
65
#生存率#
67
#胸腔镜#
59