Movement Disorders:弥散成像参数可检测、预测帕金森进展
2021-11-03 MedSci原创 MedSci原创
pSN游离水在1年内增加,基线游离水与临床运动进展相关,证明扩散成像参数对检测和预测PD进展的重要性,以及使用长TR扫描评估PD SN进展中游离水增加的重要性。
雷沙吉林作为一种治疗帕金森病(PD)的潜在疾病改善疗法,已受到关注。雷沙吉林是否能改变疾病仍有疑问。
David E. Vaillancourt等为确定1年以上雷沙吉林在帕金森病患者中是否具有的疾病改善作用。其次,评估了两种扩散磁共振成像脉冲序列,以确定评估疾病进展的最佳序列。研究成果发表在Movement Disorders杂志。

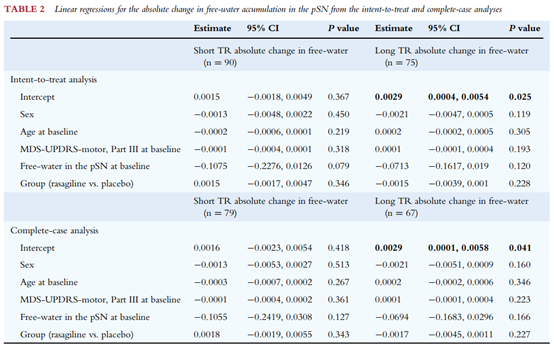
这项前瞻性、随机、双盲、安慰剂对照试验评估了12个月内服用1 mg/天的雷沙吉林对早期PD的疗效。使用两种扩散磁共振成像脉冲序列测量后黑质(pSN)自由水积聚的1年变化,一种重复时间(TR)为2500 ms(短TR;n=90),另一种TR为6400 ms(长TR;n=75)。

各组间pSN游离水累积的绝对变化无显著差异(短TR:P=0.346;长TR:P=0.228)。两组之间未发现任何次要临床结果的显著差异。

长TR,而非短TR,数据显示pSN游离水在一年内显著增加(P=0.025)。运动障碍学会统一帕金森病运动功能评定量表第三部分在1年内显著增加(P=0.009),pSN中的基线游离水与运动障碍学会统一帕金森病运动功能评定量表第三部分的1年变化(P=0.004)和动作迟缓评分的1年变化(P=0.044)相关。
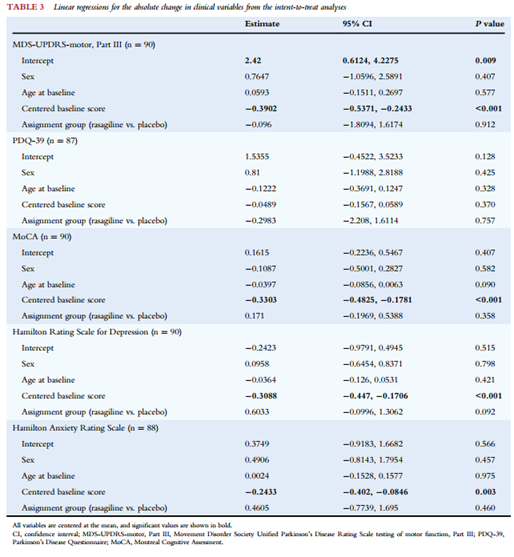
该研究未发现1年以上1毫克/天的雷沙吉林在对帕金森病有改善作用的证据。pSN游离水在1年内增加,基线游离水与临床运动进展相关,证明扩散成像参数对检测和预测PD进展的重要性,以及使用长TR扫描评估PD SN进展中游离水增加的重要性。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Dis#
75
#disorders#
68
#Disord#
63
#ERS#
65
#disorder#
71