Gastroenterology:上海交大医学院附属仁济医院揭示胰腺癌肿瘤调控新机制
2017-04-18 科学网 科学网
4月18日,记者从上海交通大学医学院附属仁济医院上海市肿瘤研究所获悉,该院“癌基因及相关基因国家重点实验室”研究员张志刚和胆胰外科主任医师孙勇伟带领团队在一项研究中阐明了胰腺癌肿瘤微环境中神经递质5-羟色胺(5-HT)系统的存在及其失调现象,证明了5-HT通过调控有氧糖酵解促进胰腺癌细胞在代谢应激条件下的生长,进而促进胰腺癌的恶性进展。该论文提供了神经递质系统
4月18日,记者从上海交通大学医学院附属仁济医院上海市肿瘤研究所获悉,该院“癌基因及相关基因国家重点实验室”研究员张志刚和胆胰外科主任医师孙勇伟带领团队在一项研究中阐明了胰腺癌肿瘤微环境中神经递质5-羟色胺(5-HT)系统的存在及其失调现象,证明了5-HT通过调控有氧糖酵解促进胰腺癌细胞在代谢应激条件下的生长,进而促进胰腺癌的恶性进展。该论文提供了神经递质系统对肿瘤调控作用的直接证据,进一步诠释了肿瘤的系统性调控理念。相关研究成果已发表于国际著名的医学杂志《胃肠病学》。
据课题负责人孙勇伟介绍:胰腺癌(PDAC)是目前人体中恶性程度最高的消化恶性肿瘤,诊断和治疗都很困难,其发病率和死亡率近年来明显上升,5年生存率小于6%,是预后最差的恶性肿瘤之一,号称“癌中之王”。胰腺癌最典型的的特征就是结缔组织增生,致密的间质成分可以达到肿瘤组分的90%,与其他肿瘤有所不同,癌细胞的快速分裂和生长需要大量能量,癌细胞通常依靠分解葡萄糖来获取能量。这就导致胰腺肿瘤细胞血供少,营养缺乏。那么胰腺癌细胞如何在这种极端的生存条件下继续充分利用这些有限的能量来源,保持生长从而完成自己的恶性生物学功能呢?
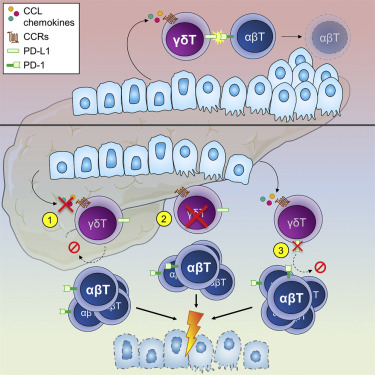
经过4年多的努力,张志刚带领团队找到了影响这一环节的重要因素:肿瘤微环境中紊乱的5-HT系统。即肿瘤细胞自身来源的5-HT通过自分泌作用于HTR2B受体,活化下游信号通路,增加了肿瘤细胞在代谢应激条件下的有氧糖酵解,为细胞的生长提供了大量的原料。其中,HTR2B受体的抑制剂SB204741能够显着抑制KPC和PDX模型中胰腺癌细胞的生长。同时,HTR2B 受体的抑制剂已进入肺动脉高压的临床实验,因其安全性较好,有可能作为胰腺癌治疗的一种候选药物。
张志刚表示,“我们的研究发现了一个胰腺癌能量利用的法宝,并且阐明了它的作用机理。令人兴奋的是,当我们剥夺了胰腺癌的这一法宝时,它的生长被显着抑制了。更加有意思的是,针对这一法宝的药物已开始用于肺动脉高压治疗的临床实验,因此我们的研究为胰腺癌的治疗提供了“老药新用”的新策略,这将大大缩短研究成果进入临床实验的时间,为胰腺癌的治疗提供新的治疗方向。”
据悉,肿瘤是一种多病因的、多基因参与的、以局部组织异常生长为特征的系统性疾病,是机体-器官-组织系统性调控失常的病变。肿瘤微环境中一些重要的调节分子,如糖皮质激素、儿茶酚胺、乙酰胆碱、皮质类固醇、免疫分子以及微环境中大量存在的细胞外基质蛋白,会影响肿瘤发展的各个层面,如肿瘤的发生、免疫逃逸和侵袭转移等,这也提示了神经-激素-分泌蛋白等组成的微环境分子网络在恶性肿瘤的演变过程中扮演着重要角色。
专家认为,这项研究成果具有重要的临床转化意义,对胰腺癌治疗效果的提升及相关患者的预后改善均有积极作用,将为今后广大胰腺疾病患者带来更多福音。
原始出处:
Jiang SH,Li J,Dong FY,et al.Increased Serotonin Signaling Contributes to the Warburg Effect in Pancreatic Tumor Cells under Metabolic Stress and Promotes Growth of Pancreatic Tumors in Mice.Gastroenterology.2017 Mar 14. pii: S0016-5085(17)30271-8. doi: 10.1053/j.gastro.2017.03.008.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#医学院#
40
#AST#
49
#GAS#
61
#Gastroenterol#
0
义榜样的力量,学习的榜样。
83
谢谢分享,很有启发意义!
103
谢谢分享,吸纳了
88
#仁济医院#
64
#Gastroenterology#
57
#上海交大#
63