Nature:靶向MET治癌——生物版“阿喀琉斯之踵”
2015-05-25 佚名 生物谷
近日,来自比利时的科学家在著名国际学术期刊nature在线发表了一项最新研究进展,他们发现肝细胞生长因子受体MET在中性粒细胞趋化以及发挥杀伤活性方面具有重要作用,但通过药物靶向MET治疗癌症的治疗效果可能因MET在中性粒细胞中的作用而部分抵消。 原癌基因MET的突变或异常表达与多种肿瘤的发生有关,同时MET信号途径的组成型激活对于肿瘤生长和存活具有重要作用。有研究发现MET不仅
近日,来自比利时的科学家在著名国际学术期刊nature在线发表了一项最新研究进展,他们发现肝细胞生长因子受体MET在中性粒细胞趋化以及发挥杀伤活性方面具有重要作用,但通过药物靶向MET治疗癌症的治疗效果可能因MET在中性粒细胞中的作用而部分抵消。
原癌基因MET的突变或异常表达与多种肿瘤的发生有关,同时MET信号途径的组成型激活对于肿瘤生长和存活具有重要作用。有研究发现MET不仅在癌细胞中表达,在肿瘤相关的间充质细胞中也存在表达,但MET表达在肿瘤相关的间充质细胞中究竟发挥什么作用仍不清楚。
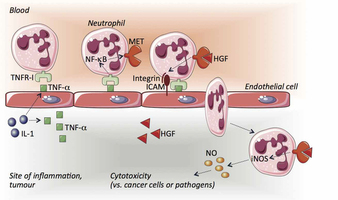
在该项研究中,研究人员发现MET对于中性粒细胞应答干细胞生长因子,产生趋化行为以及发挥细胞毒性具有重要作用。在小鼠中性粒细胞中删除Met会促进肿瘤生长及转移,这一表型与原发肿瘤和肿瘤转移灶中中性粒细胞浸润下降具有相关性。同时,MET对于中性粒细胞在大肠炎,皮疹和腹膜炎等疾病中的渗出也是非常必要的。
随后,研究人员对其中的机制进行了深入探究,他们发现在小鼠和人类中性粒细胞中MET的表达会受到肿瘤来源的TNFα以及其他炎症刺激的诱导,而这种诱导作用对于中性粒细胞跨越活化的内皮细胞以及在肝细胞生长因子刺激下产生诱导型一氧化氮合酶都是有帮助的。因此,由中性粒细胞释放的HGF/MET依赖性一氧化氮能够促进癌细胞杀伤,抑制肿瘤生长和转移。研究人员又通过全身给药的方式给予小鼠MET激酶抑制剂,证明靶向癌细胞中MET的治疗获益会因阻断中性粒细胞MET的肿瘤杀伤作用而发生部分抵消。
综上所述,这项研究发现MET在中性粒细胞发挥肿瘤杀伤作用方面具有重要作用,同时提出利用靶向MET的方法治疗癌症可能会因MET在中性粒细胞中的作用而不能获得理想的治疗效果。
原始出处:
Veronica Finisguerra, Giusy Di Conza, Mario Di Matteo, Jens Serneels, Sandra Costa, A. A.Thompson, Els Wauters, Sarah Walmsley, Hans Prenen, Zvi Granot,Andrea Casazza & Massimiliano Mazzone.MET is required for the recruitment of anti-tumoural neutrophils.Nature, May 18, 2015.doi:10.1038/nature14407
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#MET#
40
#治癌#
61
#Nat#
48