NEJM:静脉血栓栓塞患者的隐匿性癌症筛查
2015-06-24 崔倩 译 MedSci原创
背景:静脉血栓栓塞可能是癌症最早期的征兆。目前,在关于无端静脉血栓栓塞症患者的隐匿性癌症筛查在实践中有巨大差异。研究人员试图评估隐匿性癌症的筛查策略,包括第一次无端静脉血栓栓塞症患者的腹部和骨盆的综合计算机断层扫描(CT)的疗效。 方法:研究人员在加拿大进行了一项多中心,开放标签,随机对照试验。患者被随机分配接受有限的隐匿癌普查(基本血液检测,胸片,和筛查乳腺癌
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
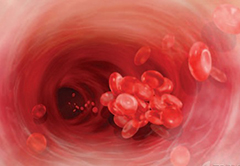








#静脉血#
50
#隐匿性#
69
值得进一步关注
128
这篇文章有一定深度
140
不错,赞一个
139
是一篇不错的文章
136
#静脉#
50
要全文
153
要看全文。
111
#癌症筛查#
77