Nature:靶向攻击p53和c-MYC可选择性清除白血病干细胞
2016-06-10 佚名 生物谷
在一项新的研究中,来自英国格拉斯哥大学、曼彻斯特大学和澳大利亚墨尔本大学的一个跨学科研究团队揭示出慢性粒细胞白血病(chronic myeloid leukaemia, CML)的阿喀琉斯之踵(即致命弱点),并且发现在小鼠体内成功地靶向攻击这种弱点和根除这种疾病的药物。相关研究结果于2016年6月8日在线发表在Nature期刊上,论文标题为“Dual targeting of p53 and

在一项新的研究中,来自英国格拉斯哥大学、曼彻斯特大学和澳大利亚墨尔本大学的一个跨学科研究团队揭示出慢性粒细胞白血病(chronic myeloid leukaemia, CML)的阿喀琉斯之踵(即致命弱点),并且发现在小鼠体内成功地靶向攻击这种弱点和根除这种疾病的药物。相关研究结果于2016年6月8日在线发表在Nature期刊上,论文标题为“Dual targeting of p53 and c-MYC selectively eliminates leukaemic stem cells”。该团队在6年多的时间里一直在开展这项研究。
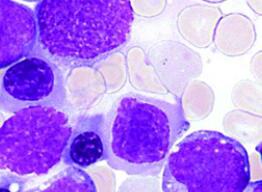
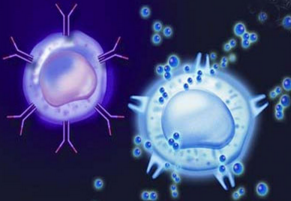
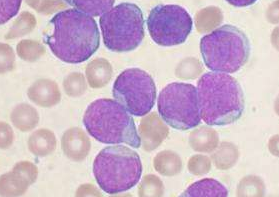
这项研究分析了慢性粒细胞白血病干细胞(CML干细胞,是一种肿瘤干细胞)和正常的造血干细胞,发现两种蛋白是CML干细胞存活的关键。研究人员随后开发出一种药物组合,这种组合同时靶向作用于这两种关键性的蛋白,杀死这些肿瘤干细胞,同时在很大程度上不会伤害正常的造血干细胞。
这个由格拉斯哥大学教授Tessa Holyoake和曼彻斯特大学教授Tony Whetton领导的跨学研究团队利用一系列技术证实这两种蛋白(p53和c-Myc)在CML中发挥关口控制器的作用。
依据精准医疗的概念(合适的药物在合适的时间在病人体内发挥合适的效果),研究人员利用CML的这种关键性的弱点,设计出一种新的治疗方法。利用移植到小鼠体内的CML干细胞开展研究,研究人员证实靶向这两种蛋白的药物组合杀死这些导致白血病的CML干细胞,有效地根除这种疾病。
这些结果对治疗急性髓性白血病(AML)和脑瘤等其他癌症产生潜在的重要影响。研究人员如今渴望在耐药性CML病人体内开展临床试验。Holyoake教授说,“我当然对这项研究中表现出的结果感到激动人心。这项研究---精准医疗起作用的一个绝佳例子---虽然处于初期阶段,但是我们获得的数据揭示出CML的两个弱点和一种潜在的药物组合疗法根除这些关键性的CML干细胞。”
研究人员在他们的研究中采用一系列技术,包括蛋白质组学、转录组学和网络分析方法。
Whetton教授说,“我们发现一种方法杀死白血病干细胞,这可能导致人们开发出一种根治而不是控制CML的方法。我们真地对我们新的蛋白质组学方法有助获得这些发现感到很兴奋。”
“对很多其他的疾病而言,我们希望我们能够利用同样的这种蛋白质组学方法为患者发现精准医疗方法。我们在曼彻斯特拥有欧洲最大的临床蛋白质组学中心,因此我们真地期待为这些研究作出贡献。”
当前的CML治疗药物是酪氨酸激酶抑制剂(tyrosine kinase inhibitors, TKIs):TKIs能够有效地控制这种疾病,但是不能治愈它。如果停止治疗的话,那么在大多数患者中,CML会复发,这就要求病人终生接受治疗。这些TKIs不仅昂贵,而且能够导致许多副作用,包括糖尿病和血管问题。正是当前CML治疗药物的成本和毒性这两个问题促使研究人员开展这项研究。
原始出处
Sheela A. Abraham, Lisa E. M. Hopcroft, Emma Carrick, Mark E. Drotar, Karen Dunn, Andrew J. K. Williamson, Koorosh Korfi, Pablo Baquero, Laura E. Park, Mary T. Scott, Francesca Pellicano, Andrew Pierce, Mhairi Copland, Craig Nourse, Sean M. Grimmond, David Vetrie, Anthony D. Whetton & Tessa L. Holyoake.Dual targeting of p53 and c-MYC selectively eliminates leukaemic stem cells.Nature.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#白血病干细胞#
72
#Nat#
62
#选择性#
56
#MYC#
70
#p53#
69
#c-myc#
82
精品文章
170
值得研究
128
新的研究进展
137
学会了
186