J Thorac Cardiov Sur:心脏病患者的福音:科学家发现Gata4或可还你一颗健康的心脏!
2017-08-16 sunshine2015 来宝网
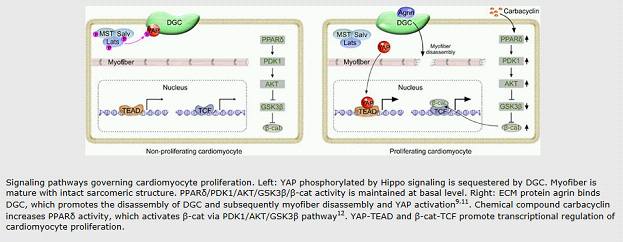
心脏病发作时,血液停止流入心脏; 缺乏氧气,心脏肌肉的一部分死亡。心肌不再生;而是用死亡组织替代由称为成纤维细胞的细胞形成的伤口,这些细胞不能帮助心脏泵。心脏减弱大多数患有严重心脏病发作的人会发展心力衰竭,这仍然是心脏病死亡的主要原因。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#THORAC#
54
#科学家发现#
49
#ATA#
61
看看学习一下知识!
73