Lancet Haematol:伊布替尼联合FCR用于初发年轻CLL患者的起始治疗:一项单臂、多中心、2期临床研究
2020-04-28 血液前沿 血液前沿
氟达拉滨、环磷酰胺和利妥昔单抗组成的FCR方案可以改善伴IGHV突变的年轻(≤65岁)化疗耐受的CLL患者的PFS。然而,不伴有IGHV突变的患者往往不能获得持久疗效。伊布替尼在CLL患者中的治
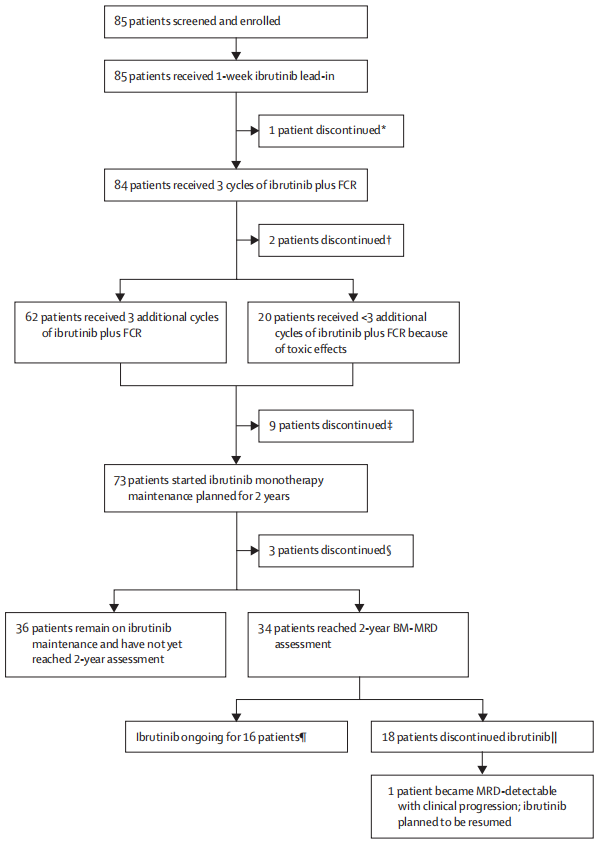
氟达拉滨、环磷酰胺和利妥昔单抗组成的FCR方案可以改善伴IGHV突变的年轻(≤65岁)化疗耐受的CLL患者的PFS。然而,不伴有IGHV突变的患者往往不能获得持久疗效。伊布替尼在CLL患者中的治疗反应不受IGHV突变状态的影响,但需要长期用药。本研究探讨了非持续使用伊布替尼联合FCR方案是否可以在耐受化疗的年轻CLL患者中产生持久的疗效。 研究设计 研究设计及入组患者:这是一项研究者发起的,多中心、开放、单臂2期临床研究,有美国的7个中心参与。入组患者为18-65岁,根据2008国际慢淋工作组(iwCLL)有治疗指征的CLL或者SLL患者,ECOG评分为0-1. 初始队列中未对预后分子进行限制,可以入组17p-或TP53异常的患者。2017年3月21号方案修改后入组的扩展队列排除了17p-的患者。 方案实施:在为期7天的起始阶段,患者仅接受伊布替尼(420mg/天)单药治疗。在第一疗程第一天给予静脉氟达拉滨(25mg/m2 d1-3)、环磷酰胺(250mg/m2,d1-3)和利妥昔单抗(375mg/m2第1疗程第1天,500mg/m2第2-6疗程第1天),联合每天口服伊布替尼
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#HAE#
81
#Lancet#
72
#多中心#
83
#2期临床#
118
#伊布替尼#
76
#EMA#
53
顶刊就是不一样,质量很高,内容精彩!学到很多
77