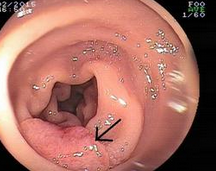
Am J Gastroenterol:内镜和手术治疗早期胃癌(非劣性研究)
2016-01-24 Mechront 译 MedSci原创
研究者对早期胃癌 (EGC)患者进行了一项研究,比较内镜切除和手术治疗的长期结局。该研究纳入了1290名内镜切除和1273名手术治疗的EGC患者。使用倾向评分匹配分析减少选择偏倚,最终涉及611对。主要结局指标:整体生存(OS)。次要结局指标:疾病特异性生存、无病生存(DFS)、无复发生存(RFS)、异时性癌症的发生、治疗相关的并发症、住院时间和30天的结局。研究数据显示,内镜切除术 vs. 手术
研究者对早期胃癌 (EGC)患者进行了一项研究,比较内镜切除和手术治疗的长期结局。
该研究纳入了1290名内镜切除和1273名手术治疗的EGC患者。使用倾向评分匹配分析减少选择偏倚,最终涉及611对。主要结局指标:整体生存(OS)。次要结局指标:疾病特异性生存、无病生存(DFS)、无复发生存(RFS)、异时性癌症的发生、治疗相关的并发症、住院时间和30天的结局。
研究数据显示,内镜切除术 vs. 手术治疗的以下方面数据分别为:10年OS:96.7% vs. 94.9% (P=0.120) (RD -1.8%, 95% CI-4.04-0.44, P非劣性=0.014),符合非劣性标准;10年RFS:93.5% vs. 98.2%(P<0.001)(RD 4.7%, 95% CI 2.50-6.97, P非劣性=0.820),不符合非劣性标准,可能是因为内镜组异时性肿瘤发生更多;并发症:9.0 vs. 6.6%, P=0.024;晚期并发症:0.5 vs. 2.9%, P<0.001。多因素COX回归分析显示以下因素可作为EGC患者OS的预测因素:年龄、合并症指数、性能指数、性别、肿瘤形态和侵袭深度。
研究结果表明,EGC患者无论选择内镜切除还是手术治疗,OS结局差不多,但手术治疗的患者在DFS、RFS和异时性RFS等方面更胜一筹。
原始出处:
Pyo JH, Lee H, Min BH,et al.Long-Term Outcome of Endoscopic Resection vs. Surgery for Early Gastric Cancer: A Non-inferiority-Matched Cohort Study.Am J Gastroenterol. 2016 Jan 19. doi: 10.1038/ajg.2015.427.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GAS#
56
#Gastroenterol#
49
#AST#
54
学习咯
142
不错,赞一个
157
这篇文章有一定深度
200
是一篇不错的文章
145
值得进一步关注
156
#内镜#
69
#手术治疗#
56