AP&T: 肝性脑病是急性失代偿肝硬化患者新发感染的独立危险因素
2022-03-09 MedSci原创 MedSci原创
肝性脑病(HE)又称肝性昏迷,是指严重肝病引起的、以代谢紊乱为基础的中枢神经系统功能失调的综合征,其主要临床表现是意识障碍、行为失常和昏迷。
显性肝性脑病 (OHE) 使多达三分之一的肝硬化患者在临床过程中的某个时间点出现肝硬化疾病进展的恶化。HE 也是肝硬化患者重复住院的主要因素,并且有很高的死亡率相关。超过 50% 的肝硬化住院患者会发生社区获得性和医疗相关感染,入院感染发生率为 25%-35%,比普通人群高 4 到 5 倍。感染与肝硬化患者进展为 HE、多器官衰竭和死亡率增加有关。然而,尽管有最好的治疗 HE 和重症监护支持,但 HE 患者的死亡风险仍然很高。本研究旨在探究 OHE 在住院期间是否易发生新发感染及其与短期死亡率的关系。
研究人员从前瞻性维护的因急性失代偿 (AD) 入院的肝硬化患者的临床数据库中筛选了 759 名合格患者。入院当天收集感染和HE数据,入院后28天评估新发感染的发生情况。EASL-CLIF 器官衰竭标准用于确定器官衰竭的存在。使用逻辑回归模型的多变量分析用于评估 28 天死亡率和新发感染的预测因子。

研究人员将患者分为四组;无OHE和感染组(n = 352);无感染但存在 OHE组(n = 221);无 OHE 但有感染组 (n = 100) 和 有OHE及感染组 (n = 86)。在多变量分析中,OHE (OR, 1.532 [95% CI, 1.061–2.300, P = 0.024]) 和进入ICU (OR, 2.303 [95% CI, 1.508–3.517, P< 0.001]) 是独立的危险因素。4组的28天死亡率分别为25.3%、60.2%、55.0%和72.1%。年龄、INR和肌酐是死亡率的独立预测因素。明显的HE、感染、凝血、肾、循环、呼吸和肝功能衰竭与较高的死亡率显着相关。
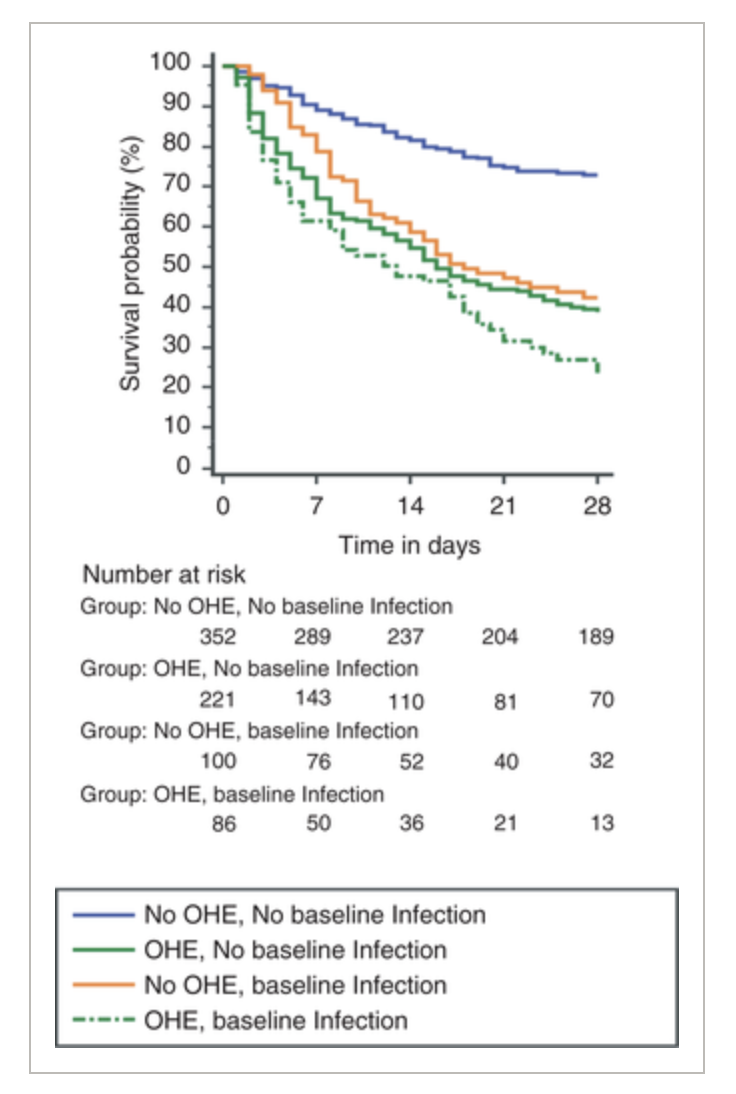
图:肝性脑病的发病率
研究结果表明 OHE 与肝硬化背景下的新发感染风险之间存在显着关系。因此,应将 OHE 患者视为新发感染的高风险,这部分患者需及早开始使用抗生素。
原始出处:
Eman Alabsawy. Et al. Overt hepatic encephalopathy is an independent risk factor for de novo infection in cirrhotic patients with acute decompensation. Alimentary Pharmacology & Therapeutics.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#脑病#
73
#独立危险因素#
85
厉害
106
厉害
85
感谢
139