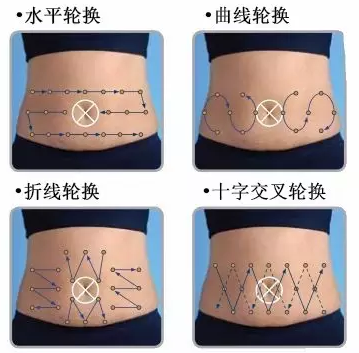
一图秒懂丨胰岛素腹部轮换注射的4种轨迹
2016-06-23 佚名 糖尿病之友
一张图,四种方法,快速学会胰岛素腹部轮换注射!关键点:1.肚脐周围5厘米,不能注射胰岛素;2.每个注射点之间至少间隔1厘米的距离。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












文章很好,非常有益
127
简单易学,指导糖尿病患者的好教程
76
#胰岛#
57
值得学习!
147
很直观,易懂
142
图很不错
170
值得学习
160