腹膜后巨大肿瘤宛若“十月怀胎”
2016-02-18 郑杨 张健 医学论坛网
腹膜后肿瘤是一类发生在腹部及盆腔腹膜后间隙的肿瘤,虽然发病率低,却涵盖了数十种组织学类型和生物学行为各异的肿瘤,加之解剖关系复杂,肿瘤常常侵犯腹膜后神经以及大血管、消化系统、泌尿系统等脏器结构,有时要求外科医生需同时具备胃肠肝胆外科、血管外科、泌尿外科甚至妇科相关的知识以及手术技术。
腹膜后肿瘤是一类发生在腹部及盆腔腹膜后间隙的肿瘤,虽然发病率低,却涵盖了数十种组织学类型和生物学行为各异的肿瘤,加之解剖关系复杂,肿瘤常常侵犯腹膜后神经以及大血管、消化系统、泌尿系统等脏器结构,有时要求外科医生需同时具备胃肠肝胆外科、血管外科、泌尿外科甚至妇科相关的知识以及手术技术。
病情回顾
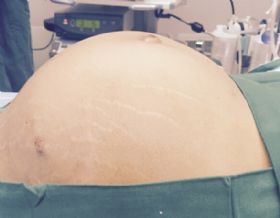
40岁的张先生,2年前发现下腹部膨隆,但并无发热、乏力,血尿、腰痛等症状,也无尿频、尿急、尿痛,腹痛等不适感,因而未予重视。1年前,张先生的腹部膨隆开始进行性增大,并出现恶心、呕吐,伴有全身浮肿。诊治前1周患者出现肢体乏力,无法站立行走,遂前往首都医科大学附属北京友谊医院急诊就诊。腹部膨隆宛如“十月怀胎”。
B超检查示腹部膨隆上至剑突,下至耻骨,两侧至腋中线
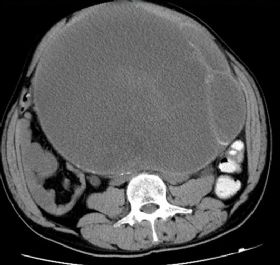
医生即刻完善相关检查,B超提示腹盆腔内囊实性肿物,双肾输尿管扩张积水。CT提示腹盆腔内见一大小约28.8cm×25.3cm巨大囊性病变,边界清楚,CT值约18-41HU,内可见分隔及壁结节,囊壁及分隔可见钙化,双肾盂、肾盏及输尿管中上段积水。急查生化提示血肌酐1600umol/L,血钾5.57mmol/L,医生立即给于患者降钾治疗,经全面分析后认为,患者肿物来源于腹膜后并严重压迫双侧输尿管,继而导致双肾积水,引发肾功能衰竭。因瘤体巨大,且已出现输尿管梗阻和肾功能衰竭。考虑到患者还年轻,如能切除肿瘤早期解除输尿管梗阻,肾功能仍有恢复可能,医生果断决定即刻收入院治疗。
入院后,医生及时给予患者血液透析,改善全身状况,并完善相关各项检查。因肿瘤较大,且可能与周围组织粘连,再者肿瘤位置较深,游离过程中极易导致骶前静脉丛出血,因此手术难度很大。有着多年的临床经验的泌尿科主任、主任医师田野,经缜密分析病情后,决定为患者尽快手术切除肿瘤。
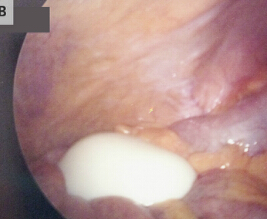
田野主任和他切除的患者的腹膜后巨大肿瘤
在完善相关术前检查和准备后,经手术室、麻醉科等专家的共同配合,田野主任和主任医师郭宇文历时3个多小时的努力,终于成功完成腹膜后巨大肿瘤的切除。术中发现肿瘤与周围组织粘连严重,根部位于骶骨尖部,分离异常困难,但仍将肿瘤完整剥离。术中未损伤小肠、结肠、膀胱、输尿管和盆腔血管神经等周围重要组织器官。患者术后恢复顺利,术后1天即可进食及下床活动,每日尿量也在2000ml 以上,肾功能逐步恢复。
田主任介绍说,腹膜后肿瘤是一类发生在腹部及盆腔腹膜后间隙的肿瘤,虽然发病率低,却涵盖了数十种组织学类型和生物学行为各异的肿瘤,加之解剖关系复杂,肿瘤常常侵犯腹膜后神经以及大血管、消化系统、泌尿系统等脏器结构,有时要求外科医生需同时具备胃肠肝胆外科、血管外科、泌尿外科甚至妇科相关的知识以及手术技术。本例巨大腹膜后肿瘤患者已出现肾功能衰竭等并发症,将严重影响其预后和生活质量,“十月怀胎”手术的成功,为该患者带来了新的生活希望。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好文章,赞
103
#腹膜后#
58
#巨大肿瘤#
68
不错的病例。期待进一步关注病理结果。
146
#腹膜#
53