Nat Commun:器官移植新进展——免疫排斥反应可被克服
2015-07-22 sunshine 译 MedSci原创
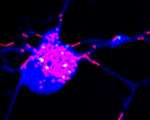
据最新的一项小鼠体内器官移植研究表明,机体对移植器官排斥的“免疫记忆”作用可能不再是一个永久的状态了,这意味着后续的移植过程可以会成功。该研究结果在线发表于Nature Communications,该研究对小鼠进行了心脏移植,并诱导其产生免疫耐受,但是在首次移植一周后二次移植前发生了免疫排斥反应。研究过程中,第二次移植的心脏顺利的被机体所接受,而且在研究过程中保持着完整的功能。 在人类器官移植中
据最新的一项小鼠体内器官移植研究表明,机体对移植器官排斥的“免疫记忆”作用可能不再是一个永久的状态了,这意味着后续的移植过程可以会成功。该研究结果在线发表于Nature Communications,该研究对小鼠进行了心脏移植,并诱导其产生免疫耐受,但是在首次移植一周后二次移植前发生了免疫排斥反应。研究过程中,第二次移植的心脏顺利的被机体所接受,而且在研究过程中保持着完整的功能。
在人类器官移植中,有些移植受体可在数周内出现免疫排斥反应,而且由于免疫记忆--免疫系统的一种警戒状态--的存在,再次移植时甚至会更快地出现排斥反应。
“尽管移植耐受暂时可被克服,但是它会似乎是一种有弹性且持久的状态,”来自伊利诺斯州芝加哥大学移植手术学教授,本研究的共同资深作者Anita Chong说道,“我们的研究结果改变了人们对移植排斥反应的免疫记忆是永久的这一看法。”
对终末期器官衰竭的患者来说,必须终身使用免疫抑制药物以防止免疫排斥反应的发生。
可以在一些患者中诱导免疫耐受-机体接受异体器官移植而不产生长期的免疫抑制作用-的产生,但是这存在一定的难度。但即使是经过长期的耐受之后,这些患者仍会被一些因素,如细菌感染,引发器官免疫排斥反应。医生们认为这可能是因为免疫系统对排斥有记忆,并防止将来器官移植的免疫耐受。
细菌一旦被清除,免疫耐受立马恢复
关于小鼠的实验室研究工作中免疫耐受可以建立,但是2个月后细菌感染给免疫耐受带来了挑战。一半的小鼠发生了器官移植排斥反应。但是研究人员发现,一旦免疫系统清除了细菌,它便可自发的恢复到早前的免疫耐受状态,并可以接受另外的心脏移植手术。
该动物实验增加了应用到人类身上的希望。“尽管小鼠和人类获得移植耐受性的方法有差异,但是维持这种耐受的机制却是相似的。”来自芝加哥大学,该研究的共同资深作者,医学教授Marisa Alegre说道,“我们的研究结果表明,对经历过器官排斥的耐受患者可以使用短期的免疫抑制药物治疗,以保护移植的器官,然后在免疫耐受恢复之后立刻停止给药。
“我们目前的工作是更加详细的了解这种耐受恢复的机制是如何发生的。”来自芝加哥大学分子医学的研究生作者Michelle Miller说道,“我们想找出是否有其他可帮助调节耐受并预防排斥记忆的机制。”
作者们在文章中总结道“他们可以为不遵循同种致敏作用的移植结果提供实验证据”,并补充道,“调节免疫记忆可以控制感染引发的器官排斥记忆。”
原始出处:
Miller ML, Daniels MD, Wang T, Chen J, Young J, Xu J, Wang Y, Yin D, Vu V, Husain AN, Alegre ML, ChongAS. Spontaneous restoration of transplantation tolerance after acute rejection.Nat Commun. 2015 Jul 7;6:7566. doi: 10.1038/ncomms8566.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
73
#Nat#
63
#排斥#
73
#排斥反应#
73
#免疫排斥#
74