Cell Stem Cell:终于抓到真凶!科学家发现帕金森病神经元死亡原因,现有药物或可治疗
2018-07-25 奇点糕 奇点网
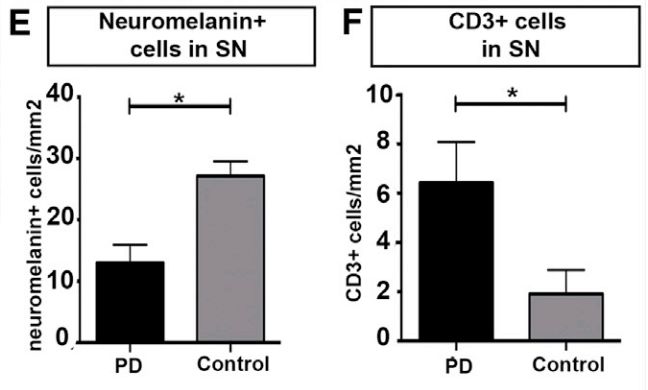
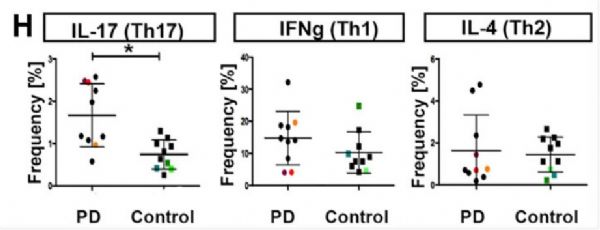
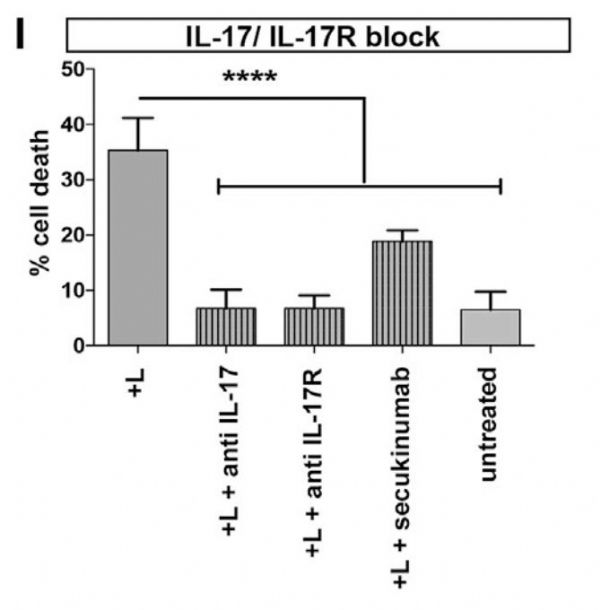
近期发表在《细胞·干细胞》杂志上的一项新研究找到了犯案“真凶”!德国弗里德里希亚历山大大学(FAU)研究者们发现,帕金森患者大脑黑质部存在大量的辅助T细胞17(Th17),而这些细胞分泌的白介素-17(IL-17)正是导致神经元死亡的关键。在利用患者诱导多功能干细胞(iPSC)构建的体外模型中,拮抗IL-17和其受体都能够阻止神经元的死亡!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#stem cell#
72
#死亡原因#
78
#CEL#
63
#Cell#
57
对MSA有用么?
108
#科学家发现#
56
#STEM#
65
向科研者致敬
127
很不错的一篇文章,为神经退行性病变治疗打开了新思路
105
谢谢,这类文章刚好是临床科研好好看的
102