ISRD & ATS 2016:白春学教授谈亚太和中国肺结节诊治指南解读与执行策略
2016-10-19 MedSci MedSci原创
上海市呼吸病研究所所长 复旦大学呼吸病研究所所长 中华医学会呼吸分会肺癌学组组长 中国肺癌防治联盟主席 亚太肺结节诊治指南制定委员会主席 白春学教授 白春学教授介绍说,所有新发肺结节在确诊之前都称之为未定性结节。对于未定性结节的处理,白春学教授提出了以下三点建议:建议1:胸部X线发现的孤立性未定性肺结节,需回顾分析既往影像学检查建议2:已稳定至少2年的未定性肺结节
2016 年10月14日~16日,由中国健康促进基金会、上海市呼吸病研究所、国际呼吸学会等主办,美国胸科协会(ATS)和复旦大学呼吸病研究所等协办,上海梅斯医学承办的“第十二届上海国际呼吸学会暨ATS联合论坛”(ISRD & ATS 2016)在上海展览中心隆重举行。14日上午,上海市呼吸病研究所所长,复旦大学呼吸病研究所所长,中华医学会呼吸分会肺癌学组组长,中国肺癌防治联盟主席,亚太肺结节诊治指南制定委员会主席白春学教授作了题为“亚太和中国肺结节诊治指南解读与执行策略”的精彩演讲。梅斯小编对白春学教授的精彩演讲进行了整理,与大家分享。

上海市呼吸病研究所所长,复旦大学呼吸病研究所所长,中华医学会呼吸分会肺癌学组组长,中国肺癌防治联盟主席,亚太肺结节诊治指南制定委员会主席 白春学教授
建议1:胸部X线发现的孤立性未定性肺结节,需回顾分析既往影像学检查
建议2:已稳定至少2年的未定性肺结节,是否需对其中高危者进行年度CT检查,要按个体化考虑。
建议3:胸部X线发现的孤立性未定性肺结节,需进行低剂量胸部CT(建议病灶薄层扫描)检查来明确其特征并评估恶性概率。
恶性肿瘤的预测模型
在目前的梅奥法预测模型中,独立的预测恶性肿瘤的因子主要有6种,包括:①年龄(OR值为1.04/年);②目前或过去吸烟史(OR值为2.2);③结节发现时至少5年前有胸腔外恶性肿瘤史(OR值为3.8);④结节直径(OR值为1.14/mm);⑤毛刺征(OR值为2.8);⑥位于上叶(OR值为2.2)。预测模型为:
恶性概率=eX/(1+eX)
X=-6.8272+(0.0391×年龄)+(0.7917×吸烟史)+(1.3388×癌症史)+(0.1274×直径)+(1.0407×毛刺征)+(0.7838×位置)
其中,e为自然对数,“年龄”为患者的年龄(岁),如果患者目前或者以前吸烟,则“吸烟史”=1(否则=0);如果患者至少5年之前有胸腔外恶性肿瘤史,则“恶性肿瘤”=1(否则=0);“直径”为结节直径(mm),如果结节边缘有毛刺,则“毛刺征”=1(否则=0);如果结节位于上叶,则“位置”=1(否则=0)。值得注意的是,对于判断恶性肿瘤的准确性,尽管模型预测结果和临床医师判断结果相近,但两者之间相关性较差,故建议依据目标人群的特点、易用性以及验证的程度来选择模型。
然后,白教授介绍了肺结节的评估方法:
1.临床信息:
采取诊断和鉴别诊断相关信息,如年龄、职业、吸烟史、个人和家族肿瘤史、治疗经过及结果。上述信息可为诊断提供重要参考意见,提高肺结节的鉴别诊断率。
2.影像学方法:
通过胸片发现的单个不确定结节者,建议应进行胸部CT检查,以便更好的描述结节(1C级)鉴别诊断。胸部CT可提高肺结节鉴别诊断率,建议根据物联网医学技术所需鉴别诊断需要,设定CT检查参数和扫描范围:
(1)扫描参数:总辐射暴露剂量≤5mSv;kVp为120;mAs≤60;机架旋转速度≤0.5;探测器准直径≤1.5mm;扫描层厚1mm;扫描间距≤层厚(3D或CAD辅助应用时需有50%重叠)。
(2)扫描范围:从肺尖到肋膈角(包括全部肺),扫描采样时间≤10s,呼吸时相为深吸气末,CT扫描探测器≥16排,不需要造影剂。
(3)肿瘤标志物:
Pro-GRP:胃泌素释放肽前体,可作为小细胞肺癌的诊断和鉴别诊断的首选标志物;
神经特异性烯醇化酶(NSE):用于小细胞肺癌的诊断和治疗反应监测;
癌胚抗原(CEA):目前血清中CEA的检查主要用于判断肺癌预后以及对治疗过程的监测;
细胞角蛋白片段19(CYFRA21-1):对肺鳞癌诊断的敏感性、特异性有一定参考意义;
麟状细胞癌抗原(SCC):对肺鳞状细胞癌疗效监测和预后判断有一定价值;
随访阶段若发现标志物进行性增高,有参考意义。
随后,白教授对不同类型的肺结节的处理方法进行了解读:
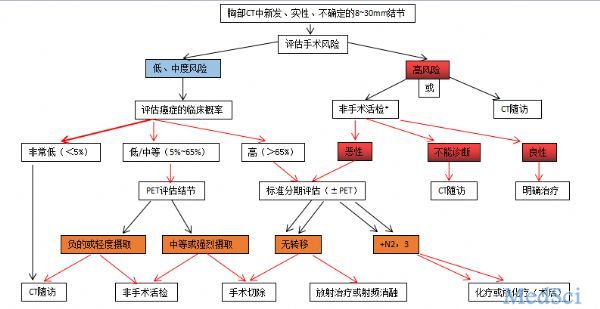
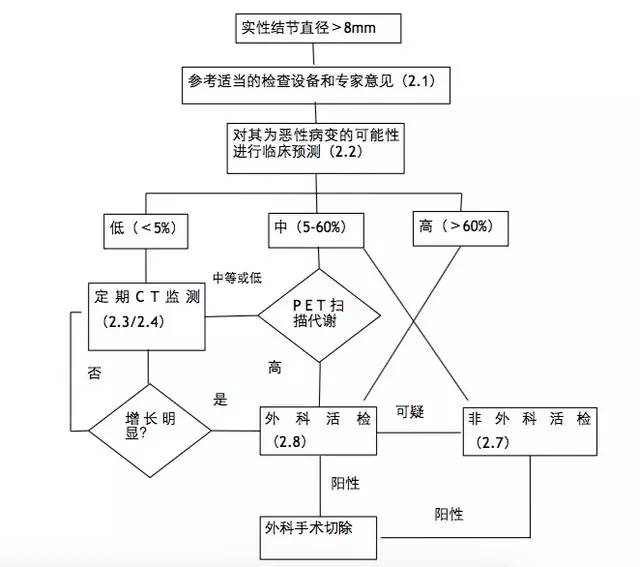
(1)对于直径8~30mm的实性结节的处理(见下图)
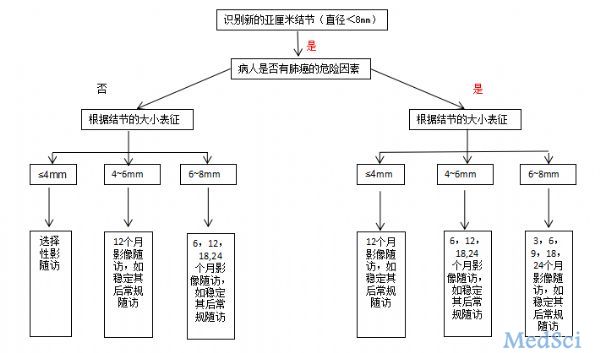
(2)对于直径<8mm的孤立性、实性结节处理(见下图)
建议1:直径≤5mm的非实性结节,根据临床和患者意愿进行年度CT随访。
建议2:直径>5mm非实性结节,每年CT随访评估至少持续3年,此后是否进行年度CT随访,需根据临床和患者意愿决定。
(2)对于孤立性部分实性(混合)结节的处理建议:
建议1:直径≤8mm的孤立性部分实性结节,建议3、12和24个月行LDCT随访,无变化者根据临床和患者意愿行LDCT年度随访,有症状或有细菌感染征象的患者,考虑经验性抗菌治疗。
建议2:直径>8mm的孤立性部分实性结节,3个月重复CT,适当考虑经验性抗菌治疗;若结节持续存在,采用非手术活检和/或手术切除进一步评估,另选择PET扫描进行术前疾病分期。
白教授还阐述了今后介入肺脏病学和未来的发展方向
白教授说,诊断和管理肺结节的方法会与时俱进,可用方法大致分为影像学、细胞学、传统的或改良的支气管镜技术、手术或非手术(如支气管镜引导下)活检等。对于肺结节来说,每种诊断方法都有各自不同的益处、风险和诊断率,如有条件,建议结合多种诊断方法,以提高诊断率和尽可能减少风险。
白教授最后总结道:肺癌的风险计算公式有限制,应考虑到亚洲肉芽肿性疾病高发,以及其它感染性因素引起的肺结节。肺结节的随访应考虑长期监测,更多使用非手术活检,较少依赖PET扫描。鼓励亚洲医生使用细节的专家共识指南,以形成对肺结节评估的一致性和可重复性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#亚太#
42
#ISRD#
58
#ATS#
54
#白春学#
67
牛人
97
#指南解读#
55
#诊治指南#
62
这个不错哦!
82