病例讨论:浮肿伴尿检异常2月余1例
2015-12-11 MedSci MedSci原创
者男性,55岁,因“浮肿伴尿检异常2月余”于2014年10月9日入院。患者2014年8月初无诱因出现双下肢间断浮肿,未予重视。2014年9月查血压为140/89mmHg,尿蛋白定量6.56g/24h,血清白蛋白18.1g/L,血清肌酐(SCr)156μmol/L,9月12日于外院行肾活检诊断“纤维样肾小球病改变伴硬化”,予保肾、利尿、抗血小板、改善微循环等处理,症状及实验室检查无明显改善,为进一步
者男性,55岁,因“浮肿伴尿检异常2月余”于2014年10月9日入院。患者2014年8月初无诱因出现双下肢间断浮肿,未予重视。2014年9月查血压为140/89mmHg,尿蛋白定量6.56g/24h,血清白蛋白18.1g/L,血清肌酐(SCr)156μmol/L,9月12日于外院行肾活检诊断“纤维样肾小球病改变伴硬化”,予保肾、利尿、抗血小板、改善微循环等处理,症状及实验室检查无明显改善,为进一步诊治收入我院。病程中患者精神、食欲、睡眠欠佳,近2个月体重下降约2kg。
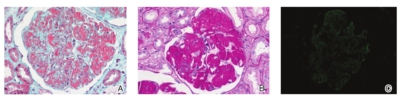
图肾活检病理A和B:肾小球系膜区弥漫增宽呈结节状,系膜区及毛细血管袢内皮下大量PAS强阳性、PASM-Masson嗜复红物沉积(PAS、Masson三色,×400);C:荧光染色示IgG+,弥漫呈颗粒状分布于系膜区及血管袢[免疫荧光(IF)×200];D和E:内皮下沉积的电子致密物呈无分支、排列紊乱的中空管状结构(电镜)。

病历摘要
患者男性,55岁,因“浮肿伴尿检异常2月余”于2014年10月9日入院。患者2014年8月初无诱因出现双下肢间断浮肿,未予重视。2014年9月查血压为140/89mmHg,尿蛋白定量6.56g/24h,血清白蛋白18.1g/L,血清肌酐(SCr)156μmol/L,9月12日于外院行肾活检诊断“纤维样肾小球病改变伴硬化”,予保肾、利尿、抗血小板、改善微循环等处理,症状及实验室检查无明显改善,为进一步诊治收入我院。病程中患者精神、食欲、睡眠欠佳,近2个月体重下降约2kg。
既往有“慢性乙型肝炎”25年,病毒无复制。“抑郁症”病史6年,曾服药治疗,已停药2年,偶有幻觉。
体格检查
体温36.7℃,血压158/105mmHg,体质指数(BMI)20.9kg/m2;正常面容,贫血貌,神志清楚,情绪低落;双下肢中度浮肿。
入院检查
尿液尿蛋白定量7.35g/24h,尿沉渣红细胞计数61万/ml(多形型),单特异性游离κ轻链191.17mg/L,λ轻链75.89mg/L,κ/λ=2.52。
血常规及血生化检查血红蛋白119g/L,白细胞计数4.9×109/mm3,血小板计数284×109/mm3。白蛋白19.1g/L,球蛋白17.1g/L,尿素氮(BUN)13.6mmol/L,SCr193.6μmol/L,尿酸(UA)451μmol/L,半胱氨酸蛋白酶抑制剂C(CystatinC)2.37mg/L,总胆固醇8.2mmol/L,甘油三酯1.5mmol/L。
免疫学检查自身抗体谱阴性,补体C30.102g/L,C40.0351g/L,IgG5.15g/L,IgA2.12g/L,IgM4.59g/L,单特异性游离κ轻链99.28mg/L,λ轻链40.81mg/L,κ/λ2.43。补体相关检查C3肾炎因子、淋巴细胞膜辅蛋白、补体H因子及抗体均正常。
超声检查心脏超声:左室舒张功能减低,左室射血分数(LVEF)为75%;双肾超声:左肾110mm×50mm×55mm、右肾122mm×42mm×61mm,皮质回声稍增强,皮髓界限欠清楚。
骨髓活检骨髓增生活跃。
肾活检病理
光镜48个肾小球,正切肾小球体积明显增大。肾小球系膜区弥漫增宽,有的呈结节状,细胞数明显减少,系膜区及毛细血管袢内皮下大量过碘酸雪夫染色(PAS)强阳性物质沉积(图A)。正六胺银-马松(PASM-Masson)染色:基膜内皮下及系膜区弥漫嗜复红物沉积(图B)。肾小管间质急性病变中度,多灶性肾小管上皮细胞刷状缘脱落,多处见等立方空泡变性。小动脉节段透明变性。刚果红染色阴性。
免疫荧光冰冻切片荧光染色IgG+(图C)、IgA+、IgM+、C3+、C1q+、κ+、λ+,弥漫呈颗粒状分布于系膜区及血管袢,IgG亚型染色示IgG1+、IgG2+、IgG3+、IgG4+,弥漫呈颗粒状分布于系膜区及血管袢。
电镜电镜下观察1个肾小球,内皮下及系膜区见大量密度不均、结构疏松的中高密度电子致密物分布,电子致密物呈无分支、排列紊乱的中空管状结构,管状物直径约16~20nm,中空直径12~17nm,长度290~810nm(图D和E)。电子致密物挤压血管袢,致袢腔狭小甚至闭塞,系膜区系膜细胞及基质明显减少。多处近端肾小管上皮细胞刷状缘脱落,胞浆内见大量脂性空泡。
诊断分析
本例患者为中年男性,病程2个月,临床表现为肾病综合征伴肾功能损害,肾外有贫血、低补体血症;肾活检光镜改变为毛细血管袢基膜内皮下大量PAS强阳性、Masson染色嗜复红物沉积,并呈结节状改变,免疫荧光为多种免疫球蛋白及补体在肾小球广泛沉积,初步诊断考虑异常物质沉积导致的肾小球肾炎。
通过临床病史及实验室检查可初步排除狼疮性肾炎(LN)、乙型肝炎病毒相关肾损害、冷球蛋白血症肾损害、华氏巨球蛋白血症、纤维连接蛋白肾小球病等疾病的诊断。
进一步的电镜观察发现,肾小球毛细血管袢基膜内皮下大量密度不均的中高密度电子致密物沉积,高倍镜观察到电子致密物具有排列不规则、直径16~20nm、中空直径12~17nm、长度290~810nm的中空管状物结构。
最后诊断免疫管状肾小球病(ITG)。
讨论
ITG由施瓦茨和刘易斯于1980年首次报道,光镜下病理形态学改变以膜增殖性病变最常见,可见系膜区和外周袢类似透明变性样的物质沉积,部分患者伴内皮细胞增殖、外周袢增厚分层。偶有表现为膜性病变和局灶节段硬化性病变,可伴有新月体及袢坏死。较少累及肾小管间质及血管。病变发展至后期由于肾小球硬化增多,可出现肾小管萎缩和间质纤维化。刚果红染色均阴性。
免疫病理检查常见IgG、C3阳性,呈颗粒状分布于系膜区及外周袢,部分伴有IgM、IgA弱阳性,C4和C1q仅在少数病例中呈散在分布。IgG亚型以IgG1或IgG4阳性多见,少有同时阳性,有时轻链只有单一轻链。
电镜是确诊ITG的主要依据,观察到的沉积物为中空微管状物,多数直径为30~60nm,少数小至20nm,大至90nm,微管状物一般呈平行规则排列,可出现“堆木柴”样排列,也有见微管状物排列紊乱甚至成团块。微管状物主要沉积于肾小球系膜区、基膜内皮下、基膜内,少数见上皮侧沉积,同一病例不同部位的微管状物直径大小一般一致。需与肾淀粉样变性、冷球蛋白血症、纤维性肾小球肾炎(FGP)等疾病鉴别。
肾淀粉样变性电镜下见无分支、排列紊乱的细纤维丝,直径为8~12nm,可分布于肾小球系膜区、毛细血管袢基底膜的上皮侧、内皮下,包曼囊壁、肾间质、肾小管基底膜及血管壁。
冷球蛋白血症肾损害患者的肾小球内中空微管状物通常排列无序,常见一些杆状、纤维状、弯曲状和指纹样结构。FGP电镜下观察见无分支、无序排列的纤维丝,直径10~30nm,纤维丝还分布于肾小球基膜内、内皮下和上皮侧,少数病例见纤维丝分布于肾小管基底膜和管周毛细血管壁上。
本例患者电镜下观察到较多无序排列的纤维丝,直径也与FGP的类似,但纤维丝均具有中空管状结构,因此仍应诊断为ITG。
小结
ITG临床罕见,主要表现为尿检异常伴高血压,多数患者伴肾功能损害,部分患者可能伴有血液系统疾病,对药物治疗反应差,预后不佳。
ITG形态学改变多为膜增生性肾小球肾炎(MPGN),超微结构见中空微管状结构平行排列。本例为非增殖性病变,以微管状免疫球蛋白广泛沉积于肾小球为特征,中空微管状物为无序排列,系首次报道,需与FGP等疾病相鉴别。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#病例讨论#
67
值得收藏
100
…………
135
#尿检#
68
病例讨论很关键
149
病例讨论,也说明临床病理的复杂性,一些普通的症状,背后可能是复杂的病因,非常值得我们临床重视
116