PLoS Biol:特殊蛋白来帮忙 不用手术也能治疗心脏疾病
2016-08-14 佚名 生物谷Bioon.com
作为世界头号杀手的冠状动脉病可以限制并且阻断血管,最终切断向心脏的氧气供应,近日一项刊登于国际杂志PLoS Biology上的研究报告中,来自中国华中科技大学等机构的研究人员通过研究发现,一种利用蛋白AGGF1的新型疗法或可成功治疗小鼠的急性心脏病发作,AGGF1是一种可以促进血管发生的特殊蛋白质
图片来源:medicalxpress.com
作为世界头号杀手的冠状动脉病可以限制并且阻断血管,最终切断向心脏的氧气供应,近日一项刊登于国际杂志PLoS Biology上的研究报告中,来自中国华中科技大学等机构的研究人员通过研究发现,一种利用蛋白AGGF1的新型疗法或可成功治疗小鼠的急性心脏病发作,AGGF1是一种可以促进血管发生的特殊蛋白质,研究者指出,这种疗法的效益依赖于自体吞噬(自噬)过程,自噬是一种移除受损或不被机体所需的细胞结构的正常机体破碎过程。
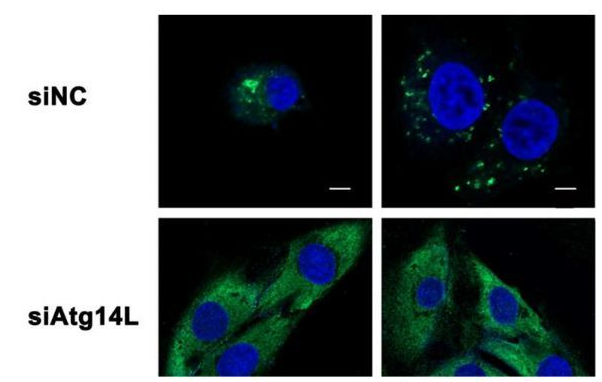
治疗性血管生成(therapeutic angiogenesis)是一种利用机体自身的因子来生长出血管的新型实验疗法,其可以作为一种内源性的过程绕过被阻断的老血管来发挥作用,文章中研究者Qing Kenneth Wang等人就对小鼠和人类机体中的蛋白AGGF1作为治疗因子的潜力进行了深入研究。血管是由内皮细胞生成,首先研究者检测了AGGF1对人类内皮细胞的效应,AGGF1暴露的早期反应可以诱导自噬过程,而自噬过程往往可以通过分子标志物以及细胞形态学的特性改变被检测到,当研究者观察利用AGGF1进行治疗的小鼠心脏时他们发现,并不仅仅是内皮细胞,心脏中其它类型的细胞也会对自噬过程产生反应。
为了检测AGGF1诱导的自噬过程和血管发生过程之间的关联,研究者利用可以抑制自噬过程的药物来进行深入研究,当利用这些药物治疗暴露于AGGF1的内皮细胞时,研究者发现,早期阶段的血管生成就会被阻断,这就意味着,自噬过程对于AGGF1介导的血管发生是必需的。当研究者创造出携带Aggf1基因单突变或双突变的小鼠时,他们发现,没有任何AGGF1的小鼠往往会在胚胎时就会死去,而大约60%的小鼠都有着完整的拷贝,然而这些小鼠却可以存活到成年期,而且其机体心脏中自噬的水平降低了。
随后研究人员对心肌梗塞的小鼠模型进行研究,他们发现,小鼠在心肌梗塞后其损伤的心脏组织中AGGF1蛋白的水平会增加,而这很有可能是损伤组织中的缺氧所介导的;心肌梗塞后利用外部AGGF1疗法进行治疗就可以增加存活期超过两周及四周小鼠的数量。研究者报道说,相比急性心肌梗塞但未接受AGGF1治疗的小鼠而言,AGGF1治疗就可以诱导自噬过程和血管发生,增加存活的心脏细胞的数量并且降低心脏结疤;同时研究人员还鉴别出了一种名为JNK的关键分子调节器,其可以介导由AGGF1进行的自噬过程的诱导,阻断JNK的药物就可以抑制这种自噬过程,而且通过药物或基因突变来阻断自噬过程需要移除AGGF1促进血管发生和心肌梗塞后心脏修复的能力,这就再次阐明了自噬过程在介导AGGF1有益效应过程中所扮演的关键角色。
最后研究者总结道,揭开自噬过程和治疗性血管生成背后的分子机制对于我们开发治疗冠状动脉疾病和心肌梗塞的新型疗法或将提供更多研究数据和希望。
原始出处:
Qiulun Lu , Yufeng Yao , Zhenkun Hu, Changqing Hu, Qixue Song, Jian Ye, Chengqi Xu, Annabel Z. Wang, Qiuyun Chen, Qing Kenneth Wang.Angiogenic Factor AGGF1 Activates Autophagy with an Essential Role in Therapeutic Angiogenesis for Heart Disease.PLoS Biol.doi:10.1371/journal.pbio.1002529
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biol#
64
#Bio#
76
文章很好值得关注
78
新思路,好
80
谢谢分享,,,,
104
值得学习
98
一个吻值得
75
继续学习
57
继续关注
54
好好学习一下
49