ACC 2014:球囊扩张式瓣膜治疗主动脉瓣狭窄或更优(CHOICE研究)
2014-04-01 小田 译 医学论坛网
2014年美国心脏病学会年会(ACC 2014)公布的CHOICE研究表明,在经导管主动脉瓣置换术(TAVR)治疗的高危主动脉瓣狭窄患者中,与应用自膨式瓣膜相比,应用球囊扩张式瓣膜可增加器械操作成功率。研究论文3月30日在线发表于《美国医学会杂志》(简称JAMA)。ACC大会演讲现场 研究共纳入241例严重主动脉瓣狭窄并适用于经股动脉TAVR术治疗的高危患者,这些患者被随机分为接受自膨式瓣膜(1
2014年美国心脏病学会年会(ACC 2014)公布的CHOICE研究表明,在经导管主动脉瓣置换术(TAVR)治疗的高危主动脉瓣狭窄患者中,与应用自膨式瓣膜相比,应用球囊扩张式瓣膜可增加器械操作成功率。研究论文3月30日在线发表于《美国医学会杂志》(简称JAMA)。
ACC大会演讲现场
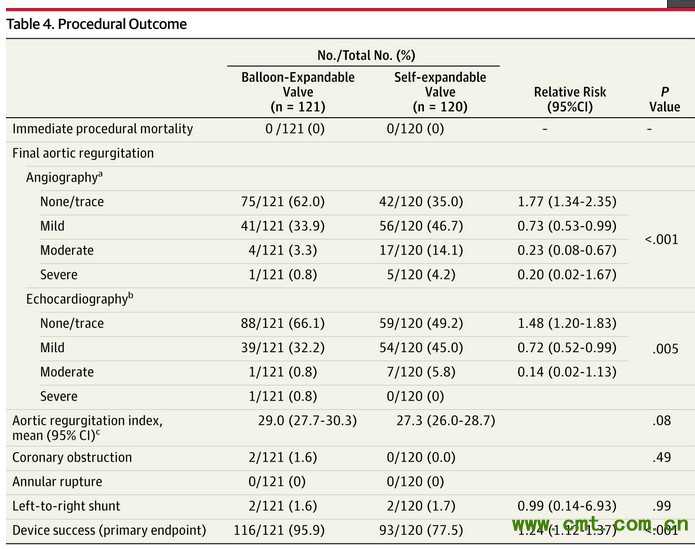
研究共纳入241例严重主动脉瓣狭窄并适用于经股动脉TAVR术治疗的高危患者,这些患者被随机分为接受自膨式瓣膜(120例)或球囊扩张式瓣膜(121例)置换术治疗。结果显示,自膨式瓣膜组和球囊扩张式瓣膜组中分别有93例和116例患者被成功置入瓣膜[相对危险(RR)为1.24,P < 0.01]。
研究者表示,造成这种差异的原因为以下两点:球囊扩张式瓣膜组的患者超过轻微剩余主动脉瓣返流频率显著降低(4.1%vs 18.3%;RR 0.23;P < 0.001),且较少需要置入超过1个瓣膜(0.8%vs 5.8%, P =0 .03)。
研究还显示,球囊扩张式瓣膜组和自膨式瓣膜组的30天心血管死亡分别为4.1%和4.3% (RR 0.97;P =0.99);两组患者的出血和血管并发症无显著差异;球囊扩张式瓣膜组患者较少置入新型永久性起搏器(17.3% vs 37.6%)。
研究者Mohamed Abdel-Wahab博士表示,目前经股动脉TAVR技术有两种瓣膜可供临床医生选择,之前一直没有对比这两种瓣膜有效性的结论性数据,因此,CHOICE研究具有重要意义,是首个对比这两种技术的随机化临床研究。
在JAMA的随刊述评上,E. Murat Tuzcu博士和Samir R. Kapadia博士写道,CHOICE研究部分填补了头对头比较的多中心、随机临床试验的重要需求。但他们也强调,还应继续努力弄清TAVR的获益和风险,尤其是在涉及患者特征和长期转归方面,有必要对这些革命性的器械进行再改进和持续的探索。他们还建议,像CHOICE的更多研究需要提供必要的证据质量,以确保TAVR合理应用和实现患者最佳转归。
原始出处:
CHOICE: Self-Expandable vs. Balloon Expandable Prostheses in Transfemoral TAVR Patients.ACC CardioSource Mar 30, 2014
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Choi#
53
#球囊扩张#
0
#扩张#
55
#ACC#
51
#主动脉瓣#
81
#球囊#
55
#主动脉#
62
#瓣膜#
48