脑室-心房分流术治疗儿童难治性脑积水1例
2020-02-07 许新科 李军亮 陈程 中国微侵袭神经外科杂志
对于多次脑室-腹腔(VP)分流术治疗失败的难治性脑积水,临床处理棘手。脑室-心房(VA)分流术是主要的替代治疗方法,但目前国内外报道多见于成人。广州市妇女儿童医疗中心使用VA分流术成功治疗1例多次手术失败的儿童难治性脑积水,效果不错,现报告如下。
对于多次脑室-腹腔(VP)分流术治疗失败的难治性脑积水,临床处理棘手。脑室-心房(VA)分流术是主要的替代治疗方法,但目前国内外报道多见于成人。广州市妇女儿童医疗中心使用VA分流术成功治疗1例多次手术失败的儿童难治性脑积水,效果不错,现报告如下。
1.病历摘要
1.1临床资料
女,2015年11月出生。病人9个月龄时因高热惊厥于外院头部CT发现第四脑室占位、脑积水。本院门诊头部MRI提示Blake囊肿与Dandy-Walker综合征鉴别。病人无明显呕吐、抽搐等不适,为进一步检查治疗于2016年8月第1次入院,既往史及孕产史无特殊。
入院查体:神志清,反应尚可,头围45 cm,前囟稍胀,大小3 cm×3 cm,余神经系统查体(-)。入院后行神经内镜检查确诊为Dandy-Walker综合征、脑积水,建议行VP分流术,家属拒绝,遂出院保守治疗。
2016年9月病人因反复呕吐第2次入院,复查头部MRI提示脑积水明显加重,脑脊液检查正常,遂行左侧VP分流术,术中置入强生可调压抗感染分流管(初压120mmH2O)。术后病人颅内压增高症状缓解,复查头部CT提示脑室较前缩小,分流管脑室端位置良好,顺利出院。
2017年3月病人因颅内压增高第3次入院,按压分流管阀门回弹缓慢,头部CT提示脑室扩张明显加重,脑脊液检查未见感染,考虑分流管脑室端阻塞,遂行左侧VP分流管拔除术+左侧VP分流术,拔除原来阻塞分流管并重新置入强生可调压抗感染分流管(初压120mmH2O),术后病人颅内压增高症状再次缓解。2017年9月开始,病人再次间断出现颅内压增高,复查头部CT提示脑室仍扩张明显,考虑分流不足,予逐渐下调分流压力至70mmH2O,颅内压增高症状缓解不明显。
于2017年12月第4次入院,脑脊液检查未见异常,按压分流管阀门回弹良好,腹部B超提示未见明显包裹性积液,分流不足原因不明,行VP分流管探查术,术中拔出分流管腹腔端,见体外引流良好,予还纳腹腔,术后颅内压增高症状有所缓解但1周左右再次出现。于2018年1月第5次入院,前后2次腹部平片提示分流管腹腔端呈盘绕状,未见明显活动改变,考虑腹腔端局限性包裹可能,遂行腹腔镜下分流管腹腔端探查+右侧脑室穿刺外引流术。术中见腹腔黏连,分流管周围大网膜包裹,予松解黏连,腹腔镜下证实引流通畅,滴速正常,并把分流管末端放置于肝脏膈面。
术后病人颅内压增高症状缓解,试夹脑室外引流管8h,病人再次出现前囟张力增高、烦躁、呕吐等颅内压增高症状,考虑腹腔黏连及脑脊液吸收障碍,于2018年1月22日行右侧VA分流术+左侧VP分流管拔除术,过程顺利,术后病人颅内压增高症状缓解(图1)。
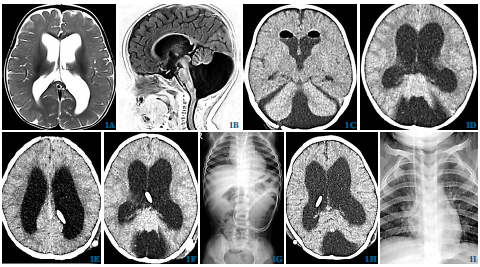
图1 VA分流术治疗儿童难治性脑积水。1A、1B首次头部MRIT2加权提示幕上脑室轻度扩张,T1加权提示小脑蚓部缺如;1C神经内镜确诊Dandy-Walker综合征术后复查头部CT;1D首次VP分流术前头部CT提示脑室扩张明显;1E首次VP分流术后头部CT提示脑室较术前缩小;1F第2次VP分流术后复查CT提示脑室再次扩张;1G腹腔镜探查前腹部平片提示腹腔端缠绕固定;1HVA分流术后头部CT提示脑室较前缩小;1IVA分流术后复查胸片提示分流管心房端位于上腔静脉接近心房处
1.2VA分流术
气管内全麻成功后,病人取仰卧位,头向左侧稍偏转并后仰,垫高肩颈部以显露甲状软骨水平的右侧颈动脉沟。取右侧颞顶部弧形切口及右侧颈部横切口,先逐层打开头部切口,颅骨钻孔,止血。打开颈部切口,显露右侧颈内静脉,向近端内侧显露右侧面总静脉。电凝硬脑膜后切开,穿刺脑室成功后,近端置入分流管脑室端,连接分流阀门后远端经皮下隧道至颈部皮下。
分流管予肝素盐水充盈后,临时阻断面总静脉切开,分流管远端经面总静脉置入右侧颈内静脉,根据术前X-线片及术中超声确定放置的深度,使得分流管远端末端至右侧心房处。确认心律及血流动力学无异常,逐层关闭切口,术毕。精神运动发育明显改善,无血栓形成、心律失常、心衰等并发症,伤口愈合良好,远期效果仍在进一步随访中。
2.讨论
随着Spitz-Holter阀门装置研发成功及投入使用,VA分流术成为治疗脑积水的重要分流术式之一。由于面总静脉解剖变异率高,经典的VA分流术操作复杂,近年来有学者提出参考颈内动脉穿刺的改良术式,手术时间明显缩短。经中国知网数据库及PubMed文献检索证实,国内外报道VA分流术均以成人为主,多数为手术技术改进及并发症的个案报道,儿童报道少见。
国内郭文龙等报道VA分流术治疗46例VP分流术治疗失败的难治性脑积水,成功率达73.9%。结合文献,作者总结本例治疗经验如下:①额角穿刺置管可减少近端脉络丛堵塞。②分流管初压的设定宜中高压,尤其对于重度脑积水病人。③重视腹腔镜探查的重要性,尤其在多次下调分流压力后脑积水缓解仍不明显时。④多次手术调整可导致失败率增加。关于VA分流术体会如下:①面总静脉的解剖体表定位约在下颌角下1 cm处。②严格无菌操作,抗生素盐水浸泡分流管。③术前结合胸片及超声等手段确定心房端位于上腔静脉接近心房处。④建议在显微镜下操作以确保操作精确,减少副反应。
综上所述,VP分流术是儿童脑积水首选的治疗方法,但术后并发症发生率仍较高,大多数需要多次手术调整,处理棘手。VA分流术是其主要的替代治疗方法,疗效确切,可以用于VP分流术治疗失败的儿童难治性脑积水。
原始出处:
许新科,李军亮,陈程,袁宏耀,林锦荣,王方宇,李方成.脑室-心房分流术治疗儿童难治性脑积水1例[J].中国微侵袭神经外科杂志,2019(01):38-39.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#脑积水#
122
#难治性#
84
#心房#
66
#脑室#
73