Nat Commun:食管鳞状细胞癌治疗新的见解
2019-04-12 cyl iNature
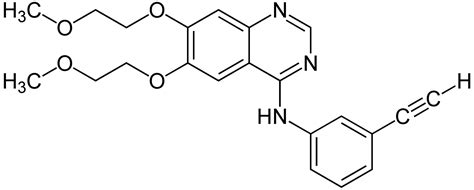
食管鳞状细胞癌(ESCC)治疗选择有限,研究表明,具有高BRCA1 / 2特征负荷的肿瘤对胰腺癌和乳腺癌中的铂疗法更敏感,这提出了ESCC中类似的突变模式可能有助于治疗不能手术的患者。此外,基于基因组学数据选择药物已经在个性化和靶向治疗的早期研究中产生了有希望的结果。一些靶向药物已用于ESCC,例如吉非替尼(EGFR抑制剂),Dovitinib(FGFR1抑制剂)和PD-L1阻断剂。然而,只有一小
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
51
#COMMUN#
44
#细胞癌#
53
#食管鳞状细胞癌#
64
#食管#
47
你们要正式
0
梅斯是骗子兑换的书吗????
110