Redox Biol:尹慧勇研究组发现脂质过氧化是冠心病的重要特征
2017-04-28 佚名 上海生命科学研究院
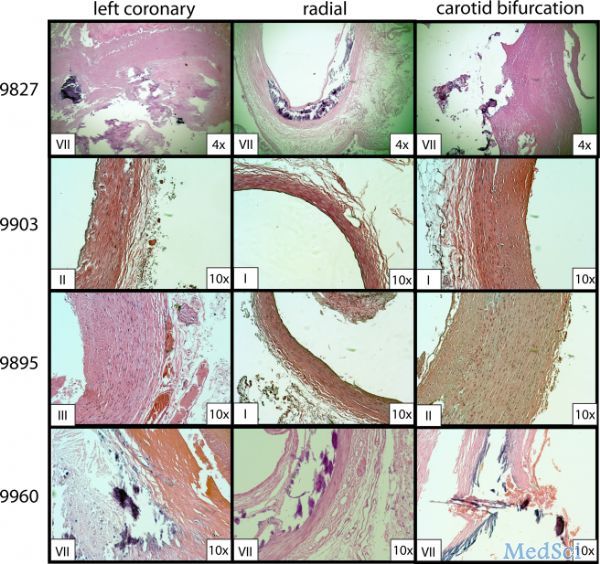
近日,国际学术期刊《氧化还原生物学》(Redox Biology)在线发表了中国科学院上海生命科学研究院(人口健康领域)尹慧勇研究组的最新研究成果Comprehensive Metabolomics Identified Lipid Peroxidation as A Prominent Feature inHuman Plasma of Patients with Coronary Heart
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Biol#
62
#Bio#
69
非常好的文章,学习了,很受益
72
学习一下谢谢分享
88
学习
85